Stages of Alzheimer’s Disease
“Memories are the threads that weave the fabric of our lives, shaping who we are and who we become.” – Elizabeth Loftus
Stages of Alzheimer’s Disease
Alzheimer’s disease is a complex condition that affects millions of individuals worldwide, impacting not only those diagnosed but also their families and caregivers. Understanding the progression of Alzheimer’s is crucial for providing appropriate care and support at each stage of the disease. In this article, we’ll explore the seven stages of Alzheimer’s Disease, highlighting the areas of the brain affected, common symptoms experienced, and available treatments for each stage.
Stage 1 – No Impairment
Area of the Brain: No noticeable changes.
Symptoms: No memory problems or cognitive decline.
Treatments: Focus on maintaining a healthy lifestyle, including regular exercise, a balanced diet, and mental stimulation.
Stage 2 – Very Mild Decline

Working Memory
Working Memory
Do you find it challenging to remember things you just learned or heard? This could be a sign of dementia.
Area of the Brain: Minimal changes, primarily in the hippocampus.
Symptoms: Occasional forgetfulness, such as misplacing keys or forgetting names.
Treatments: Continued emphasis on lifestyle factors, along with memory aids and cognitive exercises.
Stage 3 – Mild Decline

Slower Retrieval and Rapid Forgetting
Slower Retrieval and Rapid Forgetting
Finding it takes longer to recall information, and forgetting things more quickly.

Immediate Recall Difficulty
Immediate Recall Difficulty
Struggling to remember information right after learning it.
Area of the Brain: Further deterioration in the hippocampus and other regions involved in memory and learning.
Symptoms: Noticeable memory lapses, difficulty finding the right words, and challenges with planning and organization.
Treatments: Introduction of medications such as cholinesterase inhibitors to help manage cognitive symptoms, along with support from caregivers and memory care programs.
Stage 4 – Moderate Decline

Prospective Memory Challenges
Prospective Memory Challenges
Difficulty remembering to perform tasks in the future without external reminders.

Episodic Memory
Episodic Memory
Trouble remembering specific events or experiences from your past.
Area of the Brain: Significant damage in multiple brain regions, including the frontal and temporal lobes.
Symptoms: Increased memory loss, difficulty performing tasks independently, mood swings, and confusion about time and place.
Treatments: Additional medications, such as memantine, may be prescribed to manage cognitive symptoms. Occupational therapy and support services become more important for daily functioning.
Stage 5 – Moderately Severe Decline

Autobiographical Memory Changes
Autobiographical Memory Changes
Memories across your lifespan become less detailed and more vague.
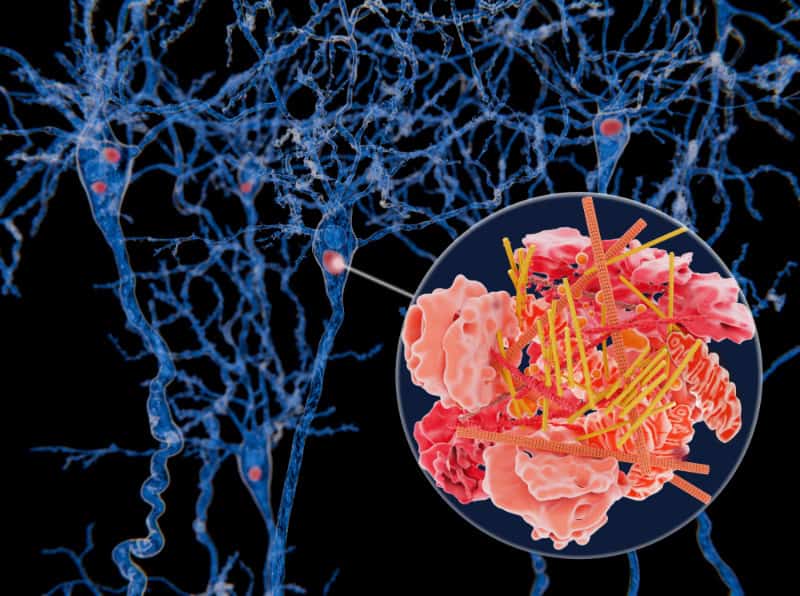
Area of the Brain: Extensive damage throughout the brain, affecting communication between neurons.
Symptoms: Severe memory impairment, inability to recall personal details, challenges with basic activities of daily living, and behavioral changes.
Treatments: Intensive support from caregivers, including assistance with personal care and supervision. Behavioral interventions and communication strategies are crucial.
Stage 7 – Very Severe Decline

Area of the Brain: Severe neuronal loss and widespread brain damage, resulting in complete dependence on others for care.
Symptoms: Loss of verbal communication, minimal responsiveness, and severe physical impairment.
Treatments: End-of-life care focuses on comfort and dignity, with a focus on pain management and emotional support for both the individual and their loved ones.
Stage 6 – Severe Decline
Area of the Brain: Severe atrophy and damage in all brain regions, leading to profound cognitive and physical decline.
Symptoms: Loss of awareness of surroundings, difficulty recognizing familiar faces, incontinence, and limited mobility.
Treatments: Palliative care focuses on maximizing comfort and quality of life. Supportive therapies, such as music and art therapy, can provide comfort and stimulation.
Bottom Line:
Understanding the stages of Alzheimer’s disease is essential for navigating the challenges and providing appropriate care and support throughout the journey. While there is currently no cure for Alzheimer’s, early diagnosis and intervention can help manage symptoms and improve quality of life for individuals and their families. With ongoing research and advancements in treatment, there is hope for a future where Alzheimer’s is more effectively managed and ultimately cured.