
Tip: Press either “Ctrl + F” or “Command+F” on your keyboard and search for a keyword related to your intervention. You will then be able to copy and paste the caption.
Tips for Defensive Documentation
Use language from the OTPF-4
State rationale and skill as an analyst
State how it relates to your scope of practice
Be thorough and leave no room for interpretation
Write so that nobody can can question your value and competence
Write so nobody can question medical necessity and justification of services the first time.
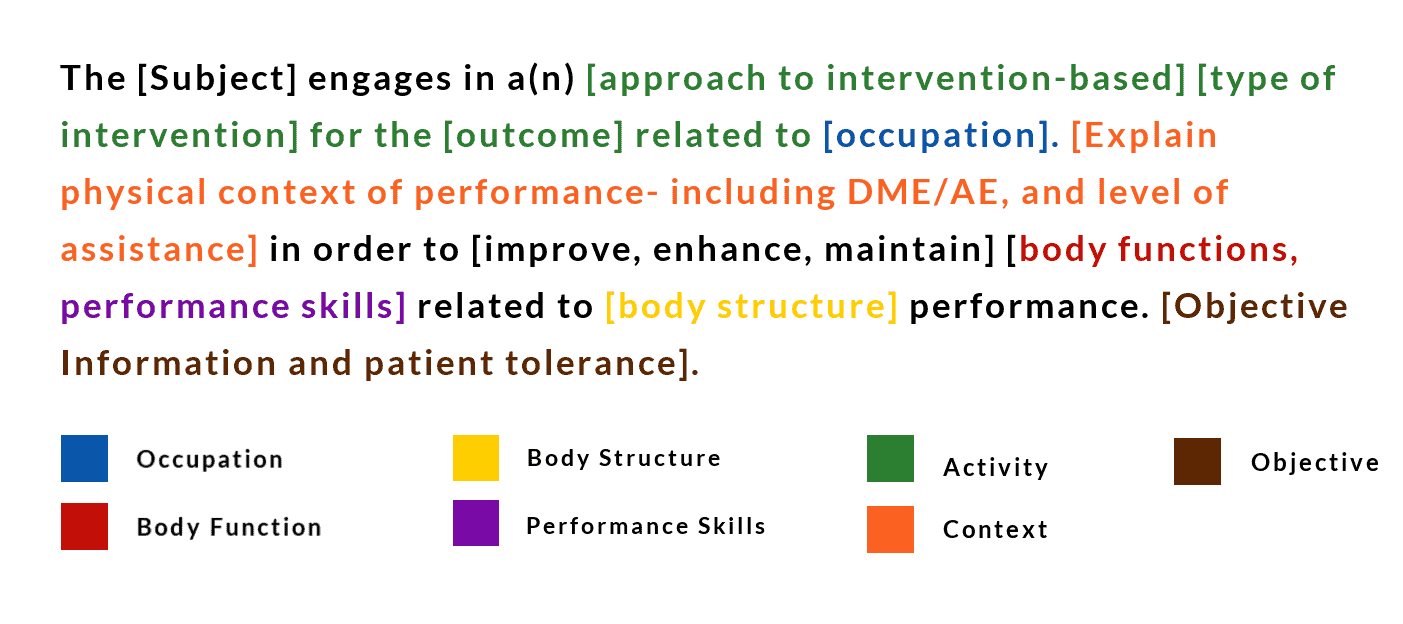
How to Build Treatment Documentation
with Language from the OT Domain
Therapeutic Activity Rationales
Billed as 97530
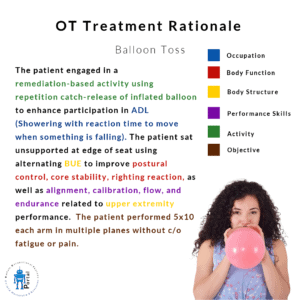
Balloon Toss
Balloon Toss
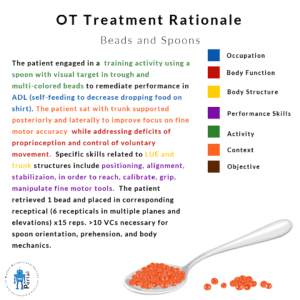
Beads and Spoons
Beads and Spoons
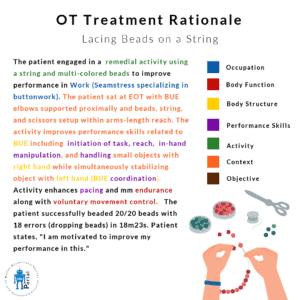
Lacing Beads on Strong
Lacing Beads on Strong
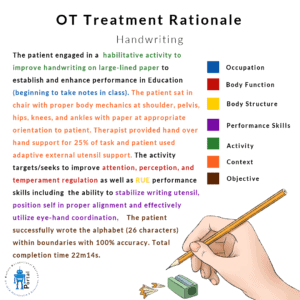
Handwriting
Handwriting
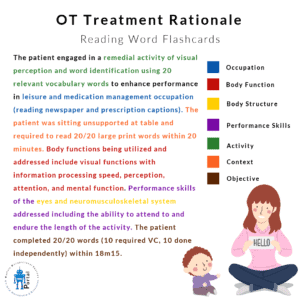
Reading word flashcards
Reading word flashcards
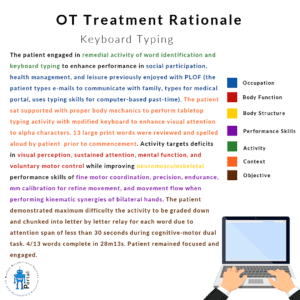
Keyboard Typing
Keyboard Typing
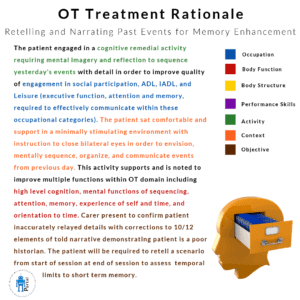
Retelling and Narrating Past Events for Memory Enhancement
Retelling and Narrating Past Events for Memory Enhancement
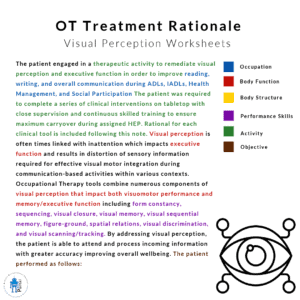
Visual Perception Worksheets
Visual Perception Worksheets
Therapeutic Exercise Rationales
Billed as 97110
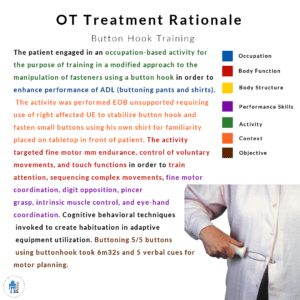
Self-Care and Community Management Rationales
Billed as 97535
Neuromuscular Re-Education Rationales
Billed as 97112
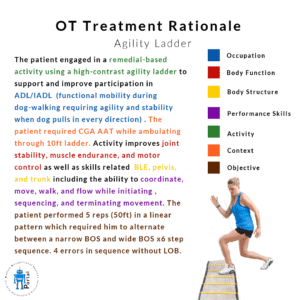
Agility Ladder Treatment Rational
Agility Ladder Treatment Rational
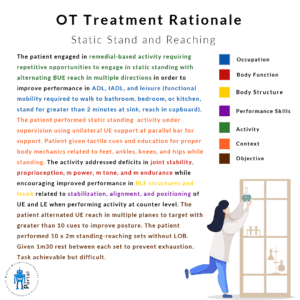
Static Stand and Reaching
Static Stand and Reaching
Backward Walking 1
Backward Walking 1
Overhead Reaching Activity
Overhead Reaching Activity
Externally Supported Digit Isolation Grasp 1
Externally Supported Digit Isolation Grasp 1
Wall Clock Multi Modal Activity
Wall Clock Multi Modal Activity
Cross Crawls
Cross Crawls
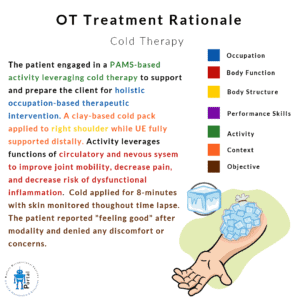
Supporting Interventions
Billed under main intervention code based on primary purpose
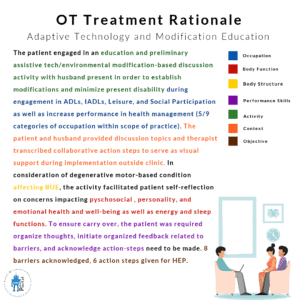
Psychosocial and Behavioral Rationales
Billed under main intervention code based on primary purpose
Self Advocacy of symptoms and self reflection
Self Advocacy of symptoms and self reflection
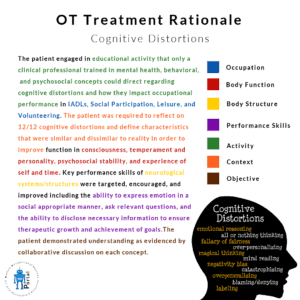
Cognitive Distortions
Cognitive Distortions
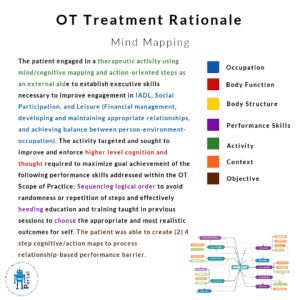
Mind Mapping
Mind Mapping
Color Picture for Self Expression and Explain
Color Picture for Self Expression and Explain
Personality Assessment and Discussion
Personality Assessment and Discussion
Time Line Intervention
Time Line Intervention
Emotional Inventory
Emotional Inventory