Balance Activities for Occupational Therapy Interventions
General:
Balance Activities in occupational therapy services are unique in that the OTP is thinking about the occupational performance, future multi-context implications, and (most importantly) the source of the client’s dysfunction so that it can be remediated or restored to it’s maximum capacity. An occupational therapy practitioner should never forget that our primary role is to restore function the correct way in order to allow our client to live a least-restrictive lifestyle. We must apply the study of medicine to analyze our client’s diagnosis, the study of biomechanics and kinesiology to restore and maximize function, and the psychosocial model in order to provide a balance between the medical and social science frame of mind. THIS is occupational therapy!
Assessments to use in Evaluation and Progress Notes:
- BERG Balance Assessment
- Timed Up and Go
- 5 Times Sit to Stand
- 10ft Tandem Line
- Modified Falls Efficacy Scale
- ABC Balance Scale
Stop feeling insecure and lost.
Don't wait for BURNOUT to consume your life because there just isn't enough time to search for evidence-based occupational therapy resources and training for daily clinical treatments.
Join the BOT Portal for occupational therapy resources and receive 24/7 access to the highest quality resources designed by an experienced therapist speciically for busy, motivated, and passionate therapists and therapy assistants.
As occupational therapists, navigating the intricacies of reimbursement and avoiding duplicate services can be challenging. Whether you’re working in skilled nursing facilities (SNFs), assisted living facilities (ALFs), or outpatient settings, precise documentation and goal-setting are essential. Here’s a guide to help you understand the importance of effective documentation and how to enhance your practice, particularly when addressing balance and stability.
The Importance of Documentation
Effective documentation is the cornerstone of occupational therapy practice. It ensures that your interventions are recognized, reimbursed, and aligned with your patient’s goals. The way you document and write your goals reflects your approach as an occupational therapy practitioner. Detailed and accurate documentation not only supports reimbursement but also distinguishes your role from other healthcare providers, such as physical therapists (PTs).
Addressing Duplicate Services
A common concern among occupational therapists is the issue of duplicate services. This often arises when multiple therapists, such as PTs, are working on similar goals like improving balance for ambulation or transfers. However, it’s essential to understand that you can still bill for these functions by emphasizing your unique occupational therapy perspective. The key lies in the language you use and the details you provide in your documentation.
Leveraging SMART Goals
One effective strategy is to use SMART goals—Specific, Measurable, Achievable, Relevant, and Time-bound. On the BOT portal, there is a training course on SMART goals that is part of the Connect Mentorship Program. This course provides valuable insights into setting clear and actionable goals. Additionally, I’m updating the documentation examples with a color-coding system to highlight where and why occupational therapy fits into the remediation process. This approach helps in clearly defining your interventions and linking them to occupational outcomes.
Understanding Balance and Stability
When working on balance and stability, it’s crucial to differentiate between these two concepts. Balance involves maintaining equilibrium without movement, often requiring proprioception and postural control. Stability, on the other hand, involves using balance during movement and engaging in multi-activity occupations within context. Knowing these differences allows you to tailor your interventions more effectively.
For instance, if PTs are working on ambulation and transfers, focus on other aspects of balance and stability that support these functions. Use sensory enhancement, strength training, or proprioceptive exercises to address specific deficits. Document these interventions thoroughly, using OTPF language and linking them to occupational goals. This approach not only ensures reimbursement but also highlights the unique value of occupational therapy.
Defensive Documentation
Defensive documentation is another critical aspect. Always be prepared to justify your interventions with clear rationales. Use specific OTPF language and patient assessments, such as the ABC Confidence Scale or the Modified Falls Efficacy Scale, to support your documentation. This practice not only protects you from audits but also reinforces the breadth of your practice.
Utilizing Resources
Take advantage of available resources like the Connect Mentorship Program and the color-coded documentation system. These tools are designed to enhance your practice by providing comprehensive knowledge and practical strategies for effective documentation. Engaging with your professional network and participating in mentorship programs can also build your confidence and improve your practice.
Blog
Alzheimer’s Disease Medications for Memory
Recent advancements in Alzheimer’s treatment have led to FDA approval of several new medications for Alzheimer’s Disease and mild cognitive impairment (MCI). These developments are the result of rigorous research and clinical trials aimed at improving the quality of life for those affected by these conditions. The newly approved medications offer hope for better management of symptoms and potentially slowing the progression of cognitive decline.
One of the key focuses of recent research has been on targeting the underlying mechanisms of Alzheimer’s, such as amyloid plaques and tau tangles. These innovative approaches have shown promise in clinical trials, leading to the approval of drugs that can more effectively address these core issues. Additionally, advancements in diagnostic tools have enabled earlier and more accurate detection of Alzheimer’s and MCI, allowing for timely intervention with these new treatments.
For healthcare professionals, caregivers, and patients, staying informed about these advancements is crucial. Our latest blog article provides a look at these new medications, their mechanisms of action, and the potential impact on patient care.
The Neurological Therapist – Interview your therapist
One crucial aspect of our practice is understanding the nuances between different treatment modalities and knowing when to apply each one effectively.
Understanding the Difference: Therapeutic Exercise, Therapeutic Activity, and Neuromuscular Re-education in Occupational Therapy
One crucial aspect of our practice is understanding the nuances between different treatment modalities and knowing when to apply each one effectively.
Stages of Alzheimer’s Disease
Alzheimer’s disease progresses through several stages, each presenting its own set of challenges for both the individual and their loved ones. In the early stages, memory lapses and difficulty with familiar tasks may be subtle, but as the disease advances, symptoms become more pronounced. In the middle stages, confusion and disorientation become more frequent, and individuals may require assistance with daily activities. Finally, in the late stages, communication becomes extremely limited, and round-the-clock care is often necessary. Understanding these stages can help families better navigate the journey of Alzheimer’s, providing support and planning for the road ahead.
Warning Signs of Dementia
It is difficult to tell the difference between memory loss in normal aging and warning signs of dementia, but there are several common findings that may serve as a warning sign that something deeper may be happening than normal aging.
Early Signs of Dementia in Women
“Memory is the treasure house of the mind wherein the monuments thereof are kept and preserved”. Thomas Fuller Early signs of dementia in women:Early: This refers to the beginning stages or the initial phase of something. In the context of "early signs of dementia,"...
Traumatic Brain Injury Rehabilitation TBI
Traumatic Brain Injury (TBI) Rehabilitation and Support ServicesTBI and Concussion in TeensTBI and Concussion in AdultsWhat is a Traumatic Brain Injury (TBI)A traumatic brain injury (TBI) can occur after a fall, sport injury, motor vehicle accident, blunt force...
Lewy Body Dementia and Rehabilitation
Lewy Body Dementia and Rehabilitation Authored by Michelle Eliason, MS, OTR/L, CKTS, C.D.S.What is Lewy Body Dementia?Lewy Body Dementia (LBD) is the second most prevalent progressive neurodegenerative diagnosis causing dementia. It is second to Alzheimer's disease...
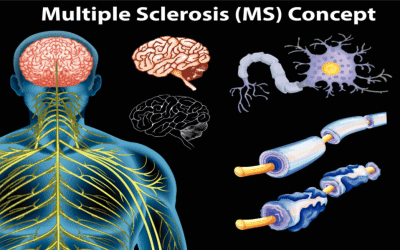
Multiple Sclerosis and Rehabilitation
Multiple Sclerosis and Rehabilitation Authored by Michelle Eliason, MS, OTR/L, CKTS, C.D.S.Common Symptoms of Multiple SclerosisMultiple sclerosis (MS) is a neurodegenerative disease affecting the central nervous system (brain and spinal cord). During the progression...
Parkinson’s Disease
Parkinson's Disease Treatment Parkinson's Disease Therapy and Management Parkinson's Disease treatment; Parkinson's Disease therapy; PD; Parkinson's Physical TherapyCommon Symptoms of Parkinson's DiseaseParkinson's disease is the second most common neurodegenerative...