Therapeutic Activities for Occupational Therapy
This page is exclusively for BOT Portal members who have joined as 6 month or 1 year members. This resource is extremely exaustive and much work time went into bringing it to you. Enjoy!
Please Note that Buffalo Occupational Therapy may benefit as an affiliate if you chose to use one of the links below. Amazon in no way endorses our business or services at Buffalo Occupational Therapy.
Instructions:

Executive Functioning and Low Level Cognition Components of Occupation Simulations
A-Z Challenge
Activity Comments
- Print A-Z Challenge, have a timer for activity completion
- Have your patient complete part 1 of the activity. Complete subjective-based questions on Part 1 after the task is completed
- Distract your client with an unrelated task for a predetermined amount of time that can be up to the length of the session (examples: mobility-based activities, social discussion, a different executive function activity)
- Complete Part 2 of the activity and the corresponding subjective based questions for your daily note
Sample Documentation
The patient completed a 2-part attention, working memory, and information processing speed worksheet in which he was challenged to write 26 places from A-Z – Subject: [Household items]. The patient completed part one within [3m39s]. The patient was delayed in recalling written items by approximately [10 mins] as he was engaged in other cognitive tasks. The patient recalled [20/26 items] within [3m 58s].
Main Idea Worksheet
Product
Use recent news articles, segments from patient-specified books, simple short stories, etc.
Activity Comments
- Obtain digestible paragraphs/short stories to read to your client – consider beforehand how you might need to grade the stories
- Ensure you have read through the paragraphs and have highlighted the main ideas for yourself
- Read at a slow pace. Repeat if necessary (also keeping track of prompts given, number of times you repeated the story, etc)
Helpful Hints:
- To grade down: Read fewer sentences to decrease the amount of details
- To grade up: adding a component of interference after the reading such as digit reversals or unrelated social conversation
Complete as a dual task! Does your patient have difficulty with delayed recall? Read the story, explain to your patient that they will need to remember key details/main ideas and state them AFTER they complete a motor component such as tandem walking or a pattern on the agility ladder
Sample Documentation
The patient engaged in an executive functioning based activity to address components of executive dysfunction and motor dysfunction impeding his ability to engage in social participation effectively. Social participation is one of the 9 domains of occupational therapy and therefore must be addressed through therapeutic activity to fulfill the therapeutic responsibility. The patient was required to listen to a paragraph of structured narrative without distraction and subsequently state the main idea of the content and [3 specific details] that led to the classification of the main idea to improve working memory, auditory processing, and auditory memory as well as verbal delivery of the information with special attention on inflection, tone, expression, and phonetics of response. The patient performed [4 of 5] of the intended paragraphs while using [therapeutic silence for [10 seconds]] between each response.
Adding Numbers to Numbers PDF
Activity Comments
- Print out (and laminate for convenience!) Numbers Executive Function 1 or 2
- Have a timer ready
- Write in the calculations for the patient on the left side of the paper (e.g +1, +3, -4, -2, etc)
- You can write a new calculation for each row or have them complete multiple rows with the same calculation
Helpful Hints:
- To grade up: Remove the visual cue of the calculations. Say to your patient, “We are going to complete an activity to help improve calculation and speed of information processing. Please add 3 to every other row starting with the first row and subtract 4 from every other row starting with the second row. Complete the calculation in your head and only say the number one you have added or subtracted.”
- Complete as a dual task. Tape the sheet to your clinic’s wall and have the patient complete the task while maintaining balance on a foam pad or a rocker board. You can also coordinate movement to each digit. For example, have your patient complete 1 standing march while simultaneously stating a digit
- This activity also works on visual scanning and visual attention!
Sample Documentation
The patient engaged in an executive function, visual motor, and gross motor activity requiring the patient to scan [3 rows] of 25 digits from left to right while [adding 2 to each digit]. The patient performed this task a total of [three times], each with increasing difficulty to focus, and calculate. The task was purposed to increase attention to task with multiple distractions in the immediate physical environment, refine the patient’s ability to multi-task, and improve the patient’s ability to complete cognitive task while under time constraints.
Attention to Detail – Immediate Recall
Product
Use recent new articles, segments from patient-specified books, simple short stories, etc.
Auditory Memory – Attention to detail 1
Auditory Memory – Attention to detail 2
Auditory Memory – Attention to detail 3
Auditory Memory – Attention to detail 4
Activity Comments
- Print, print and laminate, or pull up an attention to detail worksheet on your iPad or tablet
Helpful Hints:
- Complete as a dual task! Does your patient have difficulty with delayed recall? Read the story, explain to your patient that they will need to remember key details and answer questions AFTER they complete a motor component such as tandem walking or a pattern on the agility ladder. Your patient’s brain will be tasked with retaining details that you read while also concentrating on a balance task – this is great for balance and cognition!
Sample Documentation
The patient engaged in a multi-modal auditory memory and functional cognition task requiring alternating attention and the ability to process [2] alternating short [4-paragraph] stories read at [1 paragraph] intervals at a slow pace immediately followed by [unrelated social conversation] and subsequent completion of [18/18 questions] regarding both stories, the patient was then required to recall details of the initial story using echoic/auditory memory in the recall process. The patient was able to correctly answer [13/16 questions] correctly demonstrating good improvement and excellent therapeutic potential to reach goals.
Alternating Attention, Auditory Memory, and Information Processing
Product
Use recent new articles, segments from patient-specified books, simple short stories, etc.
Auditory Memory – Attention to detail 1
Auditory Memory – Attention to detail 2
Auditory Memory – Attention to detail 3
Auditory Memory – Attention to detail 4
Activity Comments
- Queue up your informational text or an attention to detail sheet
- Be prepared with what your “interference” or “delay” will be
Helpful Hints
- Interference of delay to address recall as well as alternating attention could look like: the completion of digit reversals, math equations, or engaging in unrelated social conversation. The goal is to pull their attention away from the original task, engage them in something unrelated and challenge their ability to return to that first task with success – this requires A LOT of cognitive flexibility!
With any of the cognitive tasks found in these pages remember – challenging yet achievable! Work with the client to find their just right challenge
Sample Documentation
The patient engaged in an activity requiring numerous elements of short term memory, attention to detail, alternating attention, delayed recall, and extrapolation. The patient was given [1 to 2] 2-sentence statements with specific details and then required to correctly answer 4/4 questions about each statement. The patient was able to successfully answer [100% of the questions x 8 statements.]
Attention to Detail with Interference
Product
Use recent new articles, segments from patient-specified books, simple short stories, etc.
Auditory Memory – Attention to detail 1
Auditory Memory – Attention to detail 2
Auditory Memory – Attention to detail 3
Auditory Memory – Attention to detail 4
Activity Comments
1. Print, print and laminate, or pull up an attention to detail worksheet on your iPad or tablet
2. Identify your “interference” this could be categorization, unrelated social conversation, the completion of exercises, or another cognitive task!
Helpful Hints:
Complete as a dual task! Does your patient have difficulty with delayed recall? Read the story, explain to your patient that they will need to remember key details and answer questions AFTER they complete a motor component such as tandem walking or a pattern on the agility ladder. Your patient’s brain will be tasked with retaining details that you read while also concentrating on a balance task – this is great for balance and cognition!
Sample Documentation
The patient engaged in an activity requiring numerous elements of short term memory, attention to detail, alternating attention, delayed recall, and extrapolation. The patient was given [1 to 2] 2-sentence statements with specific details, then required to participate in an unrelated executive functioning activity of high-level categorization naming [15 items] beginning with a specific letter, and then required to correctly answer [5/5] questions about each statement.
The patient was able to successfully answer [100% of the questions x 4 statements], but demonstrated progressive difficulty with categorization and cognitive flexibility with each trial.
T1 – [4/4 , 1:39m naming]
T2 – [4/4 , 2:02 m naming]
T3 – [3/3 , 5m04s naming]
Stopped at 4 due to onset of cognitive fatigue
Information Cards – Auditory Memory
Product
Activity Comments
- Select cards you would like to use with your clients, ensure the ones you have selected you have read through
- Be prepared to read them multiple times if necessary. Use leading prompts – help your patient extrapolate
Helpful Hints:
Complete as a dual task! Does your patient have difficulty with delayed recall? Read the story, explain to your patient that they will need to remember key details and answer questions AFTER they complete a motor component such as tandem walking or a pattern on the agility ladder. Your patient’s brain will be tasked with retaining details that you read while also concentrating on a balance task – this is great for balance and cognition!
Sample Documentation
The patient engaged in executive function enhancement activity requiring selective attention on the therapist-read information segment of [3-4 sentences] with subsequent answering of [3 questions] requiring problem solving, interpretation, and extrapolation of meaning. This task addressed attention deficits, executive functioning deficits of extrapolation, auditory recall, working memory, and overall short term memory function. The patient correctly answered completed [6/8 trials] and did not have s/s of cognitive fatigue throughout this seated task.
Auditory Memory with Executive Function
Product
Use recent new articles, segments from patient-specified books, simple short stories, etc.
Auditory Memory – Attention to detail 1
Auditory Memory – Attention to detail 2
Auditory Memory – Attention to detail 3
Auditory Memory – Attention to detail 4
Activity Comments
- Queue up your informational text or an attention to detail sheet
- Be prepared with what your “interference” or “delay” will be
Helpful Hints
- Interference of delay to address recall as well as alternating attention could look like: the completion of digit reversals, math equations, or engaging in unrelated social conversation. The goal is to pull their attention away from the original task, engage them in something unrelated and challenge their ability to return to that first task with success – this requires A LOT of cognitive flexibility!
- With any of the cognitive tasks found in these pages remember – challenging yet achievable! Work with the client to find their just right challenge
Sample Documentation
The patient engaged in a multi-modal auditory memory and functional cognition task requiring the processing of [3] alternating short [4-paragraph] stories read at a slow pace immediately followed by the requirement followed by [unrelated social conversation] and subsequent completion of [18/18] questions regarding both stories, the patient was then required to recall details of the initial story using echoic/auditory memory in the recall process. The patient was able to correctly answer [13/16] questions correctly demonstrating good improvement and excellent therapeutic potential to reach goals.
Auditory Memory – Numeric Extrapolation
Product
Activity Comments
- Have your worksheet pulled up on your iPad or tablet or have it printed out
- Decide how many elements you will add to this activity –
Use a whiteboard with magnetic numbers and letters. After reading a paragraph, have the patient select each number he/she remembers from the whiteboard and place them in order. Keep track of how many times your patient requires the paragraph to be read through in order to collect all of the numbers. Once the numbers have been pulled from the whiteboard, go through each number and prompt the patient to recall what each number represented with the paragraph.
Play music in the background for an additional challenge
Implement a delay by having the patient engage in or complete an unrelated task (digit reversals, unrelated social conversation, categorization, etc)
Sample Documentation
The patient engaged in a multi-modal auditory memory and numeric extrapolation from narrative activity requiring the processing of [3] alternating short [4-sentence paragraphs] read at a conversational pace immediately followed by the subsequent completion of [5/5 numeric / label elements] of the read statement. The patient found this very difficulty, but experienced improvements throughout the session:
T1 = [Required three readings to achieve 4/5 success rate]
T2 = [Required three readings to achieve 4/5 success rate]
T3 = [Required 2 readings to achieve 5/5 success rate]
T4 = [Required 2 readings to achieve 5/5 success rate]
Auditory Sequential Memory with Related or Unrelated Words
Product
Activity Comments
- Select which word worksheet you will utilize. Have it printed and laminated or pulled up on your tablet
- If this is your first time doing something like this with your client be prepared to increase or decrease the number of words in order to find their just right challenge
- Determine whether or not you will introduce a motor component to this task by way of dual-tasking
Helpful Hints:
- With PD patients we have utilized the list of unassociated words while targeting working memory and *BIG* movements. Assign your patient 4-6 unassociated words (or whatever is their tolerance), have them repeat them back to you to ensure proper retention, prompt your patient to complete 15 big claps (arms coming into full horizontal adduction and back to midline) counting each repetition out loud. After the completion of their claps prompt the patient to recall the assigned words (documentation sample below)
- Discuss internal memory strategies for better retention of words such as chunking (remembering words in pairs/groups)
Sample Documentation
- The patient engaged in an auditory sequential memory task requiring the memorization and recall of a strand of unrelated words. The task was purposed to improve short term memory, invoke attention, and engage the encoding process required for echoic memory. The patient was required to remember a [2-6 item sequence] of words that were [unrelated/ meaningful to the client (biblical terms)]. Successfully completed [2-3 word spans] [without error] after a [10 second pause], but [required 2+ trials after being asked to immediately recall 4 or more word sequences]. The patient required a rest after activity secondary to feeling “a little more tired.”
The patient completed a delayed recall activity in which he was given [x4] unassociated words and then tasked with large bilateral clapping while counting aloud to [10]. The patient successfully recalled the following: [T1: 3/3 T2: 1/3 T3: 3/4 T4: 4/4 T5: 4/4 T6: 4/4 T7: 3/4 T8: 3/4] The patient was noted to have difficulty reiterating the words and required multiple attempts before motor components.
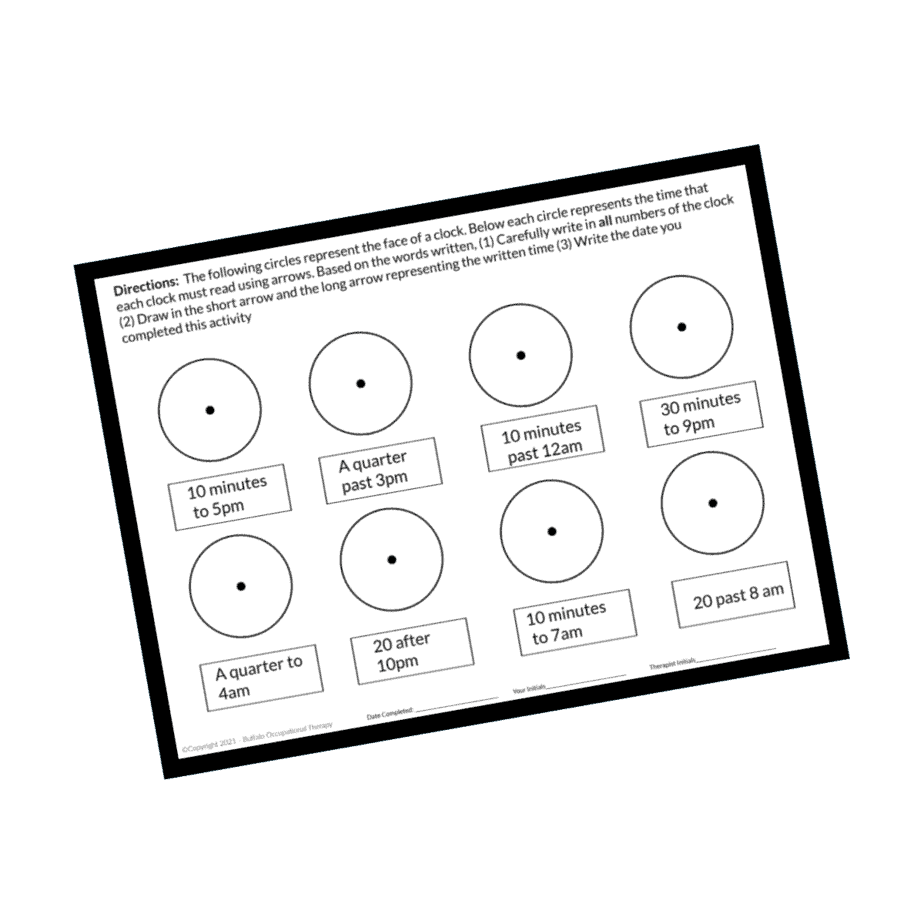
Clock Drawing : Analog to Digital
Activity Comments
- Print out time worksheets. Consider whether or not you need a couple copies for explanation and intervention as well as patient homework
- Have different colored pens/markers accessible. Writing the minutes outside of the hour markers (e.g. 1=5, 2=10, 3=15, etc) in a different color can help your patient orient to the symbolic interpretation they may be having difficulty with
- Blank sheet of paper or a whiteboard may also come in handy for additional explanation/practice
Sample Documentation
The patient engaged in a time management and time interpretation task requiring the proper translation from digital to analog time, identification of appropriate occupations for specific time, and the ability to utilize symbolic interpretation of time to convert to narrative explanation. The task worked to improve and enhance deficits in executive function (organization, regulation, orientation, and interpretation), global cognitive status and mechanisms of information recall, problem-solving, and attention, visuospatial abilities (understand visual and symbolic representations and their spatial relationships), remaining focused and utilizing selective attention to remain engaged in the task, and the ability to access semantic knowledge without prompting. The patient performed [5/10] digital-analog conversion prior to cognitive fatigue. The patient was given HEP to further promote these skills
Calendar Activity
Product
Magnetic Calendar and Magnets
Duo White board / Magnetic Calendar and Magnets
Activity Comments
- Prepare your environment for this activity. Have a flat surface to lay activity icons so your patient can scan and select them at the appropriate time
- Have previously prepared sentences to write out on a whiteboard for your patient to read one at a time
(Depending on the activity icons you have, your sentences may sound like the following) “Every Monday for the next 3 weeks you go to yoga class.” “You have two upcoming football games to attend. One on Saturday the 23rd and the other on Fridays the 29th.”
Helpful Hints:
- You can easily grade this activity up or down by what you chose to write in your sentences! Add more or less details based on your patients skills and achievability.
- Specific icons can be placed throughout the room in order to combine functional mobility, working memory, and sequencing into this activity! (e.g “Mrs Smith, we have just read the sentence and I and going to remind you that all food related icons are in the corner by the mat table and all sports and fun related icons are in the corner near the therabands and gait belts…”)
Sample Documentation
The patient participated in a visual memory and executive function-based activity utilizing a calendar to improve the ability to engage in household management which is a crucial IADL. The patient was required to review a written sentence detailing a date and an activity, retrieve a coordinating activity icon, and correctly place it on the large calendar. The patient leveraged figure ground, visual perception, executive functions, working memory, and problem solving capabilities in order to correctly place all items with [3 VSs and 1 kinesthetic cue for assistance.] The patient demonstrated difficulty orienting to the task for [5/15] trials, but was observed to have improved performance by the end.
Patient Education on Memory
Activity Comments
- Ensure that this resource will be easily accessible on your laptop or other device – knowledge is power and it’s likely that your patient has never had their injury or symptoms explained to them by a medical professional
- Be prepared with handouts if appropriate
Sample Documentation
The patient engaged in memory training to promote increased understanding and relatability of her diagnosis and therapeutic potential in order to increase internal locus of control during the therapeutic process. The education was [50% completed] discussing the encoding process and the types of memory being impacted by a traumatic brain injury will be discussed in the next session. The patient was given an assignment [to remember 10 related items using discussed internal memory tools and told she would be required to recite these 10 items without hesitation at the next visit]. The patient remained engaged throughout education and was able to offer insightful and introspective responses. Based on the material, the patient believes [her attention and working memory have been impacted the most following her injury.]
Counting Backward [Serial Subtraction]
Activity Comments
- This activity can be completed as a seated cognitive activity, used as an infererance component when completing a recall activity, or implemented as a cognitive-motor dual task
- Serial subtraction as a cognitive-motor dual task can be verbally explained and completed with our without the use of “Numbers Executive Function” worksheet
- Tape the worksheet to the wall at eye level and have the patient state the calculated subtraction out loud while simultaneously balancing on a rocker board/ foam pad/ or bosu ball
Prompt the patient to “count backward starting with 150” (true serial subtraction!) while they are completing a motor component such as tossing a large exercise ball back and forth, walking the tandem line, or standing on a rocker board
Sample Documentation
The patient engaged in counting backward exercises today as the executive function and neurological-based multi-modal activity used in conjunction with auditory memory enhancement training. Because counting forward and backward rely on canonical (Broca and Wernicke) language areas, incorporating counting activities into memory-enhancement training will allow for the activation and excitation of critical language functions affected by traumatic brain injury. Furthermore, in both forward and backward counting, studies have suggested prefrontal cortex activation which plays a critical role in the storage and manipulation of information in working memory. The patient demonstrates [moderate difficulty counting backwards between auditory memory activities as evidenced by the following outcomes:]
T1: [count 100 to 50 by 3 = 9 errors]
T2: [count 0-50 by 2 = 7 errors and slow]
T3: [count 50-0 by 3 = 9 errors and slow]
Delayed Recall with Visomotor Skills and Executive Function
Activity Comments
- Obtain both the “Numbers Executive Function” worksheet as well as an “Attention to Detail” worksheet for the memory component
- Read the sentences or paragraph, have your patient complete rows of numbers and then return their attention to the first component of this task
Helpful Hints:
- It may take you a couple of trials to assess your patient “just right challenge” – be prepared to grade this activity to your patient’s needs! This can simply be done by increasing or decreasing the difficulty of the interference task (complete more rows of numbers, have them complete multiplication rather than addition or subtraction etc)
Sample Documentation
The patient engaged in an activity requiring numerous elements of short term memory, attention to detail, alternating attention, delayed recall, and extrapolation. The patient was read a [3-4 paragraph] short story with specific details, then required to participate in an unrelated executive functioning activity, and then required to correctly answer questions about each statement The unrelated executive functioning activity required the patient to engage in an executive function, visual motor, and gross motor activity requiring the patient to scan [3 rows of 25 digits from left to right while adding 2 or 3 to each digits.] The patient performed this task a total of [two times], in between delayed recall tasks. The task was purposed to increase attention to tasks with multiple distractions in the immediate physical environment, refine the patient’s ability to multi-task, and improve the patient’s ability to dual task while under time constraints. The patient was noted to have difficulty recalling details from the story that involved numerous numbers.
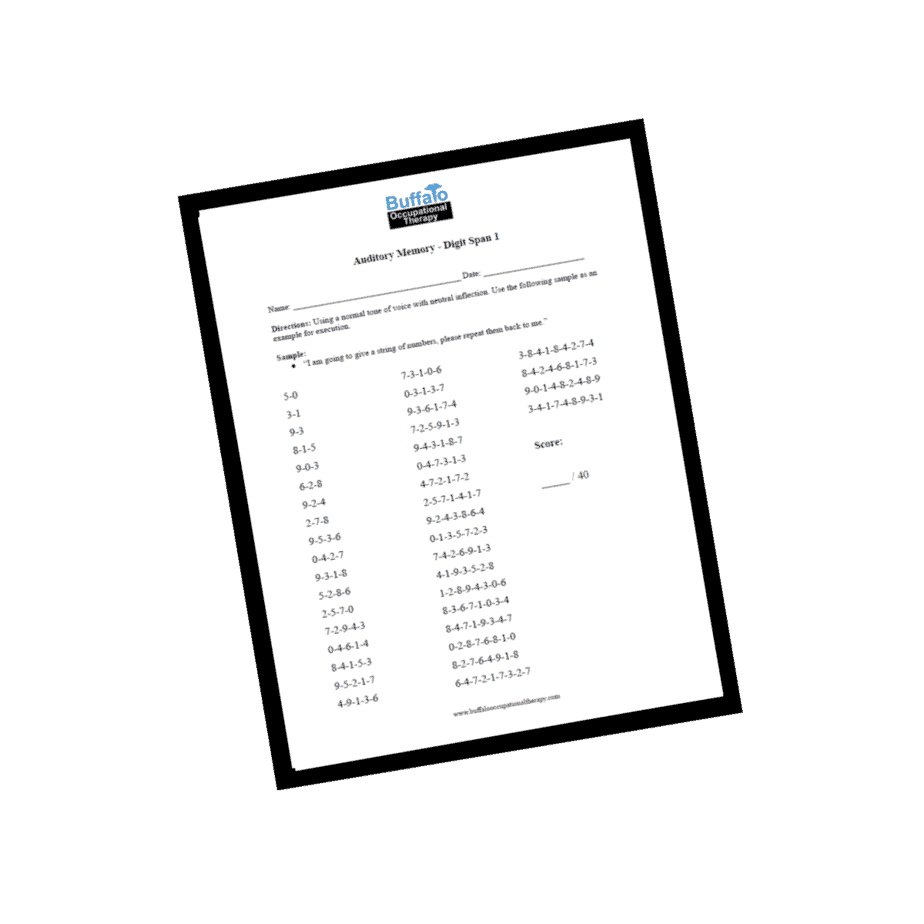
Digit Span Reversals
Product
Auditory Memory – Digit span reversals 1
Auditory Memory – Digit span reversals 2
Auditory Memory – Digit Span 1
Auditory Memory – Digit Span 2
Auditory Memory – Digit Span 3
Auditory Memory – Digit Span 4
Activity Comments
- Prepare yourself with a page of digit spans
- This can be completed as a seated cognitive activity or as a cognitive-motor dual task (add a motor component such as balancing on a foam pad or rocker board)
- State the digits with a monotone voice, slowly
Sample Documentation
The patient engaged in a digit span and registration activity for the remediation of short-term verbal memory. The patient was assigned a digit span of [5 numerical values] and measured for forward and reverse-order or backwards (also called digit reversal) recall of digit sequences. The optimal sequences are as follows: 9 digits forward, 8 backward. [7 sets] performed total with increasing information processing difficulty noted.
T1 – [No errors]
T2 – [No errors]
T3 – [1 error]
T4 – [4 errors, 5th success]
T5 – [No errors]
T6 – [3 erros, 4th success]
T7 – [5 errors]
Task terminated due to cognitive fatigue
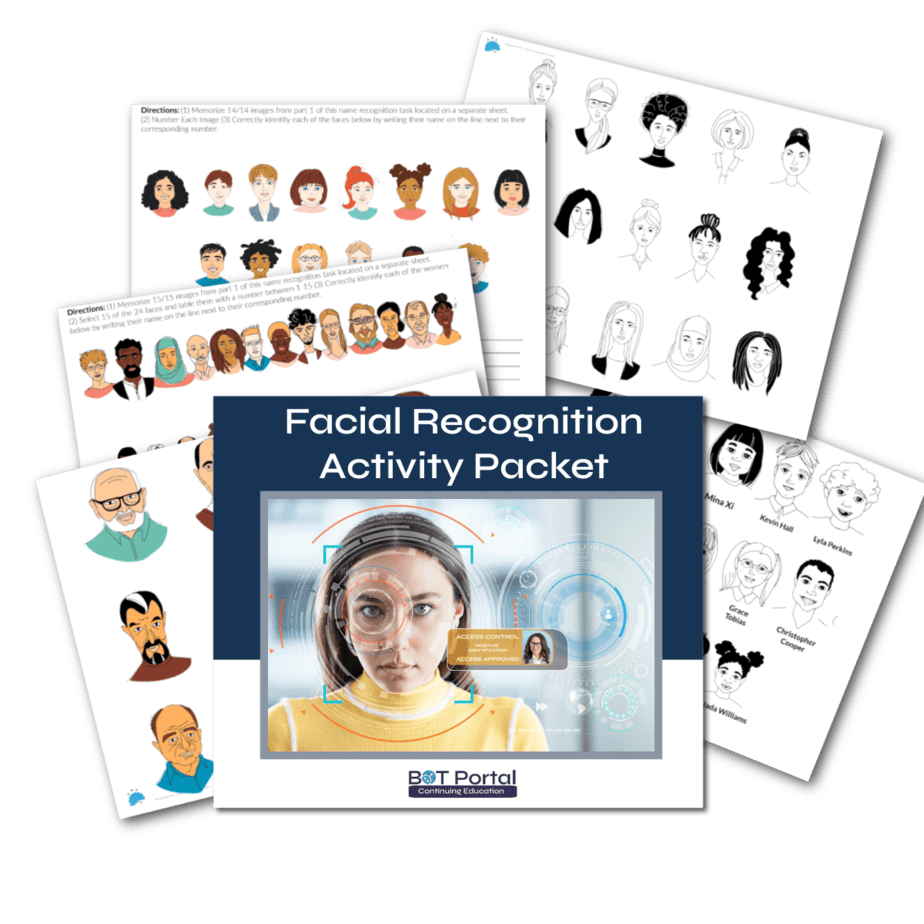
Name and Face Recognition
Activity Comments
- Print out the face recognition packet and decide which components you would like to use! The volume of this resource will allow you to provide homework for your patient for increased carry over
- This, again, can be used as a seated cognition intervention and with or without an interference task
Sample Documentation
The patient engaged in face-recognition activity to remediate and restore normal face-processing mechanisms by way of visio-cognitive training. The patient was required to remember [6/6 faces] with first and last names and make associations with each image. The patient was given [2.5 minutes] to review faces and the names were removed. The patient was able to recall [4/6 first names] before requiring a second attempt. During the second attempt, the patient was given [1.5 minutes] to review before names disappeared. At this point the patient was able to repeat [5 of 6 first and last names accurately]. Third trial, the patient was given [30 seconds] to review. During the third attempt the patient was able to successfully name the first and last names of each person.
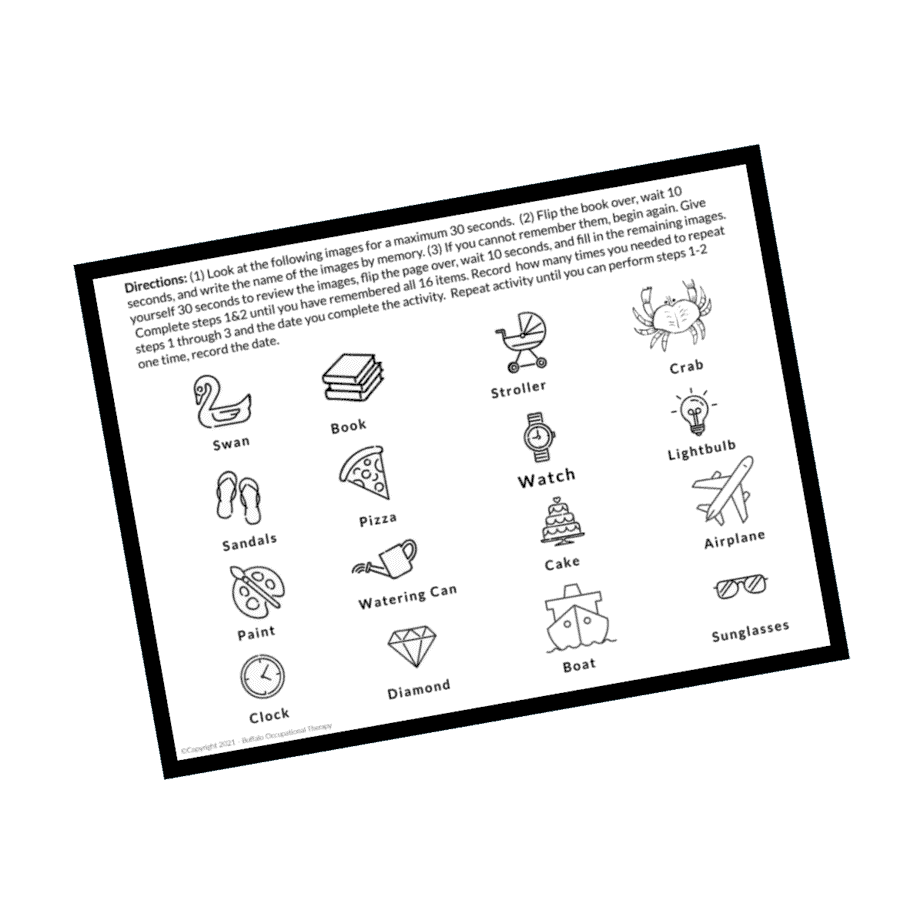
Visual Memory and Spatial Orientation
Product
Visual Memory 1
Activity Comments
- Ensure you have both sides of this activity
- Allow your patient to scan the micro images – encourage the patient to scan and recall in an organized fashion (1 row at a time, 4 corners first… etc)
- Keep time of the patient’s exposure to the pictures (measurability!)
- Allow some time for interference (start with 10-15 seconds and increase to fit your patients needs)
- Show the patient the blank piece of paper and ask them to recall what they can
Sample Documentation
The patient engaged in an activity to improve visual memory, focused and selective attention, and spatial orientation by requiring the patient to review an organized image containing [4×4] micro images and recalling those images after prompt was removed. The patient required [5 trials x 45 second] exposure to prompt in order to remember all [16 images.] The patient demonstrated alternate attention as evidenced by performing an unrelated task for [3m44s] followed by the ability to recall [4/16 elements.] This demonstrates progression to higher levels of attention.
Medication Management [Sorting and Follow Directions] Activity
Activity Comments
- Prepare the environment for this seated cognition task
- Explain to your patient the rationale behind this activity
Sample Documentation
The patient engaged in a self-management activity to improve medication adherence through cognitive remedial techniques to improve the executive function and working memory abilities of patients impacted by underlying conditions. The patient was first required to verbalize intention for activity and their meaningful connection to it. This activity used to approach superimposed executive function on fine motor skills like coordination, precision, and manipulation to improve overall functional performance in health management skills to verify independence, competence, and safety during execution. The patient was able to interpret and transfer [5 x 5-task notecards] [without assistance] [in 25m22s.]
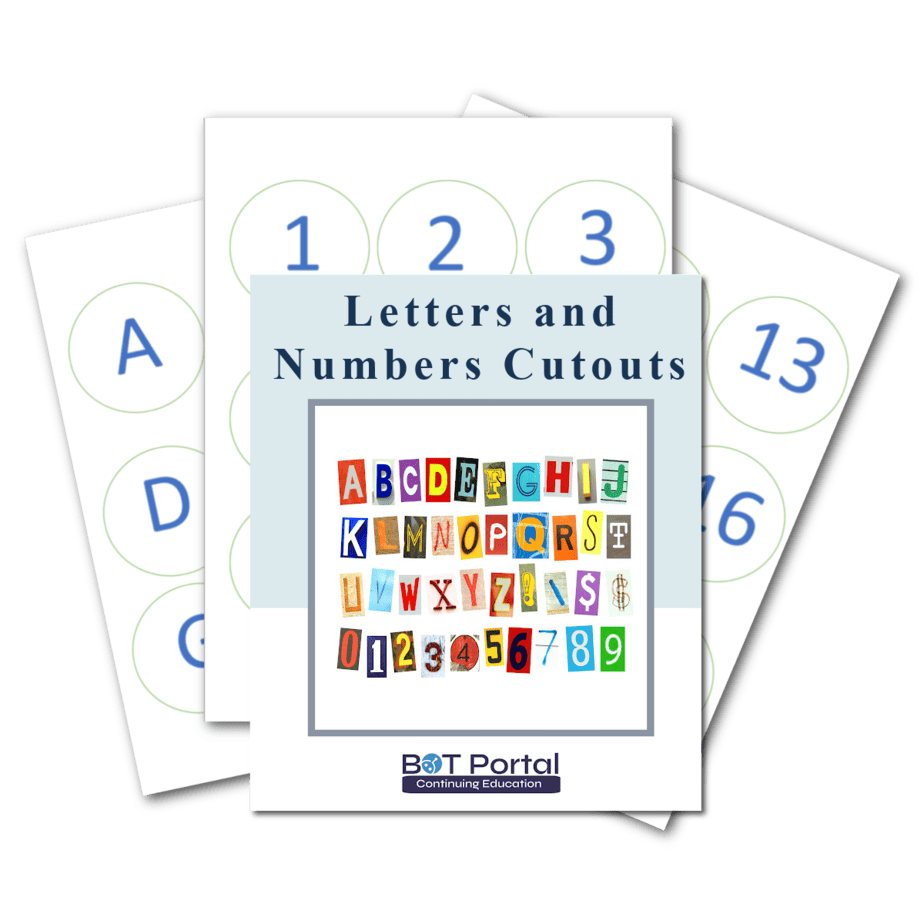
Trail Making Activity on White Board [numbers only]
Activity Comments
- Prepare the environment for this seated cognition task
- Explain to your patient the rationale behind this activity
Sample Documentation
The patient engaged in a self-management activity to improve medication adherence through cognitive remedial techniques to improve the executive function and working memory abilities of patients impacted by underlying conditions. The patient was first required to verbalize intention for activity and their meaningful connection to it. This activity used to approach superimposed executive function on fine motor skills like coordination, precision, and manipulation to improve overall functional performance in health management skills to verify independence, competence, and safety during execution. The patient was able to interpret and transfer [5 x 5-task notecards] [without assistance] [in 25m22s.]
Trail Making Activity on White Board [numbers only]
Activity Comments
- We complete this activity on a large whiteboard to emphasize visual scanning, postural alignment, and midline crossing – consider how the set up of this activity will influence your patient’s posture. Ensure proper mechanics!
- Place your numbered cutouts in a scattered fashion across the whiteboard
- Explain to your patient that they are tasked to connected each numbered circle in order with a dry erase marker
Sample Documentation
The patient engaged in an activity to address established deficits in selective attention and focus visual search speed, scanning, visuomotor coordination and communication, speed of processing, mental flexibility, working memory, and overall executive functioning. This particular activity also requires gross mobility, postural engagement, and sustained standing tolerance. The patient was required to perform a trail making activity with numerics [1-30] over a large space to encourage maximum performance of all functional deficits noted in the trail making assessment during evaluation. The patient was noted to have moderate difficulty as evidenced by [5 VCs and 2 physical gestures], but demonstrates fair potential for improvement as evidenced by motivation to complete the task. The patient required [5m42] seconds to complete this task with a goal of [less than 3 minutes] now established.
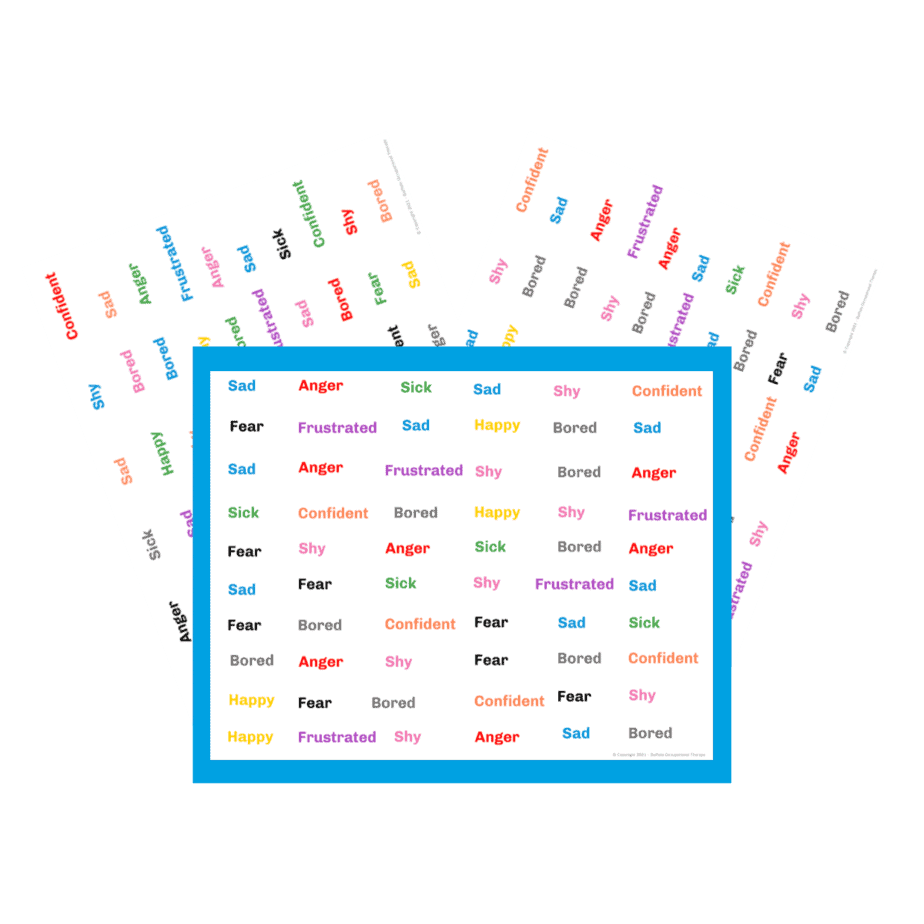
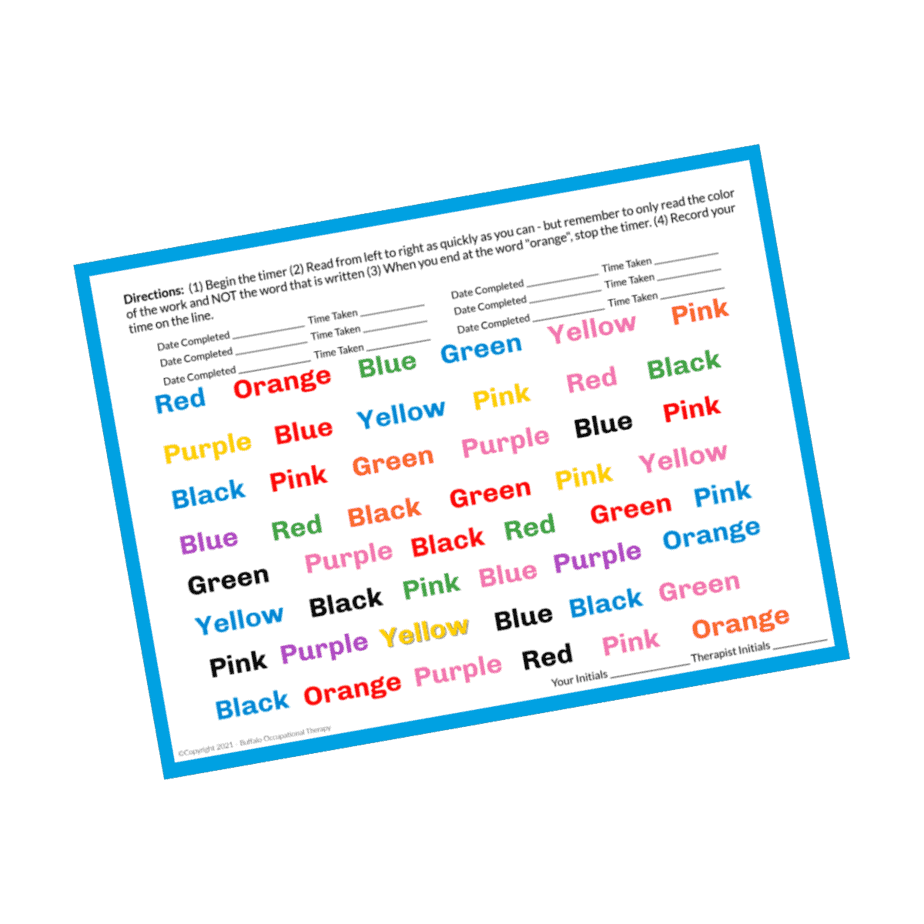
Stroop Emotions
Activity Comments
Print the STROOP
Sample Documentation
The patient was introduced to a difficult STROOP test. requiring the ability to attend, encode, store, consolidate, and retrieve new information. This STROOP requires the learned association of colors to emotions in order to later dismiss irrelevant words in order to verbalize the appropriate emotion associated with the color. Activity purposes to increase attention to tasks requiring high cognitive demand in prefrontal cortex functions. Stroop is used to assess and improve the cascade of control between neurocognitive brain functions required to exhibit cognitive control when manipulating task-relevant and task-irrelevant information. The patient must use cognitive control to overcome the tendency to read the word and base a decision on that information to prioritize processing of ink color so as to guide responding. The patient had a good understanding of the directions of this task and was able to complete this task. Because this was the initial introduction of this activity, the patient was required to read [60/60 words] [10 times] stating the color and the emotion associated with the color in order to increase and support the encoding and storing functions of new memory acquisition.
Stroop Colors
Activity Comments
Print the STROOP
Sample Documentation
The patient engaged in [2/2 trials] of a medium difficulty STROOP test. Activity purposes to increase attention to tasks requiring high cognitive demand in prefrontal cortex functions. Stroop is used to assess and improve the cascade of control between neurocognitive brain functions required to exhibit cognitive control when manipulating task-relevant and task-irrelevant information. The patient must use cognitive control to overcome the tendency to read the word and base a decision on that information to prioritize processing of ink color so as to guide responding. The patient had a good understanding of the directions of this task and was able to complete this task [objective measure to follow]. The patient reports feeling a slight heachache beginning in the back of her head and radiating to the front of her head. As well as slight pain right in the middle. She is unable to determine if this was a symptom of her vaccine or focus.
[4 Lines, 5 words per line]
T1 – 1 minute 8 (2 errors)
T2 – 34 seconds, no errors. Increased headache as the patient said she looked at words through her peripheral to avoid confusion of what was being read. The patient was educated regarding the importance of reducing visual strain during concentration, and to embrace the challenge of the activity while utilizing wellness strategies like closing her eyes, resting before continuing to the next line, taking increased time.
T3 – 44s no errors
T4 – 41 seconds no errors
T5 – 57 seconds 6 errors: “This one was taxing and I feel tired at this point.
Trail Making Activity on White Board [letters and numbers]
Activity Comments
- We complete this activity on a large whiteboard to emphasize visual scanning, postural alignment, and midline crossing – consider how the set up of this activity will influence your patient’s posture. Ensure proper mechanics!
- Place the lettered cutouts in a scattered fashion across the whiteboard
- Explain to your patient that they are tasked to connected each letter circle in alphabetical order with a dry erase marker
Sample Documentation
The patient engaged in an activity to address established deficits in selective attention and focus visual search speed, figure-ground, scanning, visuomotor coordination and communication, speed of processing, mental flexibility, working memory, and overall executive functioning. This particular activity also requires gross mobility, postural engagement, and sustained standing tolerance. The patient was required to sequence alpha-numerics [26 letters and 26 numbers] over a large space to encourage maximum performance of all functional deficits noted in the trail making assessment during evaluation. The patient was able to complete this activity in [7.20 seconds] without verbal cues or assistance.
Card Matching
Product
Activity Comments
- This activity can be done with playing cards, hand-made cards using photos of meaningful people and places, letter cards, etc.
- Have a timer ready to use.
- Arrange the cards/photos in a grid using appropriate number of cards 3×4, 5×5, etc.
- Explain how many matches you will have your patient find. You can issue a time-oriented goal (countdown) or measure how long it takes to find all matches.
Sample Documentation
The patient engaged in neurocognitive stimulation using the pelmanism system to promote visual memory, sequential processing, short term memory, reaction time, and intentional recall. Task required [6 matches with 10 second visual processing before the recall period]. The patient demonstrated the ability to successfully pair [6 matches] [in 58 seconds] with [12 errors]. This activity is designed to promote increased independence and safety while living at home, maximize functional performance during essential IADLs, and prolong quality of life.

Mobility-based Components of Occupation Simulations
Forward trunk flexion with functional reach to cones/objects of choice
Product
Activity Comments
- This activity can be completed on a mat table or in an armless chair
- Assess, through activity analysis, what movement patterns you are trying to invoke. Use the environment around you to facilitate this!
Sample Documentation
The patient engaged in dynamic sitting activity requiring forward flexion to floor level with reach outside BOS to retrieve [15/15 cones] and return to midline with trunk rotation and lateral flexion for cone placement. Movements enhance ability to center mass over BOS while seated for improved ability to don pants at floor level and increase participation in self-care. Activity enhances BUE strength, core/postural stability, and tolerance for controlled and intention movements to increase safety awareness and prevent falls d/t generalized weakness.
Reach to Floor Level
Product
Activity Comments
- This activity can be completed on a mat table or in an armless chair
- Assess, through activity analysis, what movement patterns you are trying to invoke. Use the environment around you to facilitate this!
Sample Documentation
Patient engaged in functional reach activity requiring BUE and core/trunk isometric muscle contraction while reaching to ground level with proper body mechanics, touching target (colored cone), and returning to standing posture with [CGA] [2×10 reps] in order to promote muscle strengthening, vestibular conditioning, enhanced posture, diaphragmatic breathing, and endurance for activity. Because the patient has a noted history of falls due to picking up items from floor-level, activity used to increase safety and ability to pick up items efficiently and confidently while decreasing risk for fall.
Therapy Eggs for Grasp Strength
Product
Activity Comments
- Have your patient seated at a table (consider ergonomics of hand therapy)
- Select resistance that is challenging yet achievable – ask your patient how many they think they could do
- Ensure your patient isn’t compensating higher up in the kinetic chain! Watch for shoulder abduction and trunk flexion
Sample Documentation
The patient used the flexxfix hand system to improve various functional grasp patterns to strengthen patient-stated deficits of spherical and cylindrical grasp performance during functional activities like opening jars and containers. The patient was required to use the [medium “green” resistive ball] to perform exercises activating the three mm of the thenar eminence and surrounding supporting and stabilizing structures. Activity performed with [10 concentric isotonic contractions] to full range and the [3 second isometric hold] at end range. Patient able to complete the activity but required cryotherapy for approximately [4 minutes] immediately following activity for pain management and relaxation.
Therapy Eggs for Pinch Strength
Product
Activity Comments
- Have your patient seated at a table (consider ergonomics of hand therapy)
- Select resistance that is challenging yet achievable – ask your patient how many they think they could do
- Ensure your patient isn’t compensating higher up in the kinetic chain! Watch for shoulder abduction and trunk flexion
Sample Documentation
The patient used the flexxfix hand system to improve various functional pinch patterns including tip punch, chuck pinch, and lateral pinch. The patient was required to use the [“soft” yellow egg] for tip pinch exercise and the [“medium ” red egg] for chuck and lateral pinch exercises. Activity performed with [x10 concentric isotonic contractions] to full range and the [3 second isometric hold] at end range. Therapist-initiated termination of each set at [x5 repetitions] due to threshold before at least 5/10 pain experienced vocalized by patient.
Fine motor – Bead Placing by Color
Product
Activity Comments
- Collect your beads and cups – set your patient up at a table
- Placing a towel down can help prevent beads dropping to the floor
Sample Documentation
The patient engaged in a kinetic-based therapeutic activity requiring the gathering of [30 beads (5 different colors)] be placed into designated unlabeled cups after transferring beads using alternating tip to tip pinch and placing each bead into a small target. The task elicited fine motor coordination, in-hand manipulation, and mm endurance of intrinsic muscles of the hand. Task required fine motor refinement, rotation and stabilization of the objects while isolating movement of the beads with the thumb, index and middle fingers, ring and 5th digit. The patient performed this activity with each hand and reports it is a good challenge. The cognitive component of this task required the patient to remember and recall which unlabeled cup held which color. The therapist gave the patient [4-5 colors] that the patient would need to pick up and place in sequence. The patient was able to successfully complete [5/10] trials demonstrating deceased working memory and recall as well as possible attention deficits.
Feeding Simulations – Beads and Spoons
Product
Activity Comments
- Set your patient up at a table
- While your patient is performing repetitions you should be dissecting their movement patterns to see what needs to be worked on to help with the efficiency of this ADL!
- This is a task specific activity that can be blocked practiced for motor re-learning or even with a metronome to assist in inhibiting tremors in those with PD
Sample Documentation
Patient participated in skilled intervention to increase participation in feeding and other fine motor daily living tasks. Throughout retrieval and placement activity, the patient was tasked with modulation of hand, wrist, and finger movement to maintain efficient spoon placement, pacing of self, attention to the task at hand, awareness and response to change in the placement of container, intentional focus on muscle movement and blocked repetition of activity has potential to establish new neural pathways to increase participation and carryover in feeding task. Activity simulated necessary feeding skills required and, overall, the patient demonstrated success in compensatory spoon holding technique; the patient engaged in activity for [10 consecutive minutes] with good success.
Manipulating Beads and Placing them in a Jar
Product
Activity Comments
- Collect your beads and cups – set your patient up at a table
- Placing a towel down can help prevent beads dropping to the floor
Sample Documentation
The patient engaged in a kinetic-based therapeutic activity requiring the gathering of [20 beads] into the palm of the right hand (and then left in separate repetition) with subsequent placement of each bead into a small target. The task elicited fine motor coordination, in-hand manipulation, and mm endurance of intrinsic muscles of the hand. Task requires translation, shift, rotation and stabilization of the objects within the palm space by eliciting mm involvement of the ring and pinky fingers while isolating movement of the beads with the thumb, index and middle fingers.
Functional Ambulation through Corridor
Product
Activity Comments
Helpful Hints:
- This is a great note to add any DME training to! Upwalker, canes, walkers, etc…
- If your facility allows it, consider ambulating outdoors as well for increased practice in community mobility. Traversing different terrains can bring out many deficits not previously seen
Sample Documentation
Patient engaged in functional mobility throughout the corridor. Indoor environment required intention and focus to increase spatial orientation and navigational skills, visual perceptual skills, depth perception, dynamic balance, stamina for gross movement, and the ability to incorporate ambulation aide in everyday mobility. The patient ambulated approximately [200ft] [with CGA] and no c/o of fatigue or discomfort. Activity utilized to enhance participation in independent indoor/outdoor mobility, participation in IADLs, and traversing obstacles without risk of fall.
Hula Hoop – Upper Extremity Range of Motion
Product
Activity Comments
- Seat your patient on a mat table with hip, knees, and ankles at 90°
- Habe your patient hold the hula hoop with BUE at 10 and 2 or 3 and 9 depending on the client range of motion
- While this is targeting UE ROM, it’s also challenging your patient core and postural stability
- Add a metronome to this activity to promote reaction time and neural excitation
Sample Documentation
The patient engaged in a BUE AROM, mm elongation, and generalized strengthening activity requiring him to hold the hula hoop at various points to elicit gross shoulder flexion, pronation/supination, internal/external rotation, scapular protraction/retraction. The patient performed [2×15] each movement pattern with noted fatigue at the end of sequence. Therapeutic rest offered.
Upper Extremity Metronome Training
Product
Activity Comments
Helpful Hints:
- Metronome training can be added to any functional movement pattern, therapeutic activity, or exercise
- Metronome training has been implemented and studied in many groups of individuals! From older adults, to athletes, to post CVA patients, to those with neuromuscular conditions
Metronome training improves reaction time, coordination, alertness of extremities, and concentration!
Sample Documentation
The patient engaged in seated BUE AROM kinetic activity requiring rhythmic coordination with metronome at [55BPM] in various UE functional movement patterns. Today’s session targeted shoulder flexion extension with maximum difficulty. The patient continuously offered feedback that she was not able to move either hand in conjunction to beat as her movements would either be too big or too small implying modulation deficits. The patient requires further sessions to maximize performance in this EBP. This task is purposed to address symptoms of movement initiation, coordination, and control associated with her primary diagnosis. Metronome training has been proven to increase the accuracy of the central motor impulse and therefore the impulse force of the nerve over which the command is issued. Consequently, the regulation of the skeletal muscles by the central nervous system can reinforce the coordination between agonizing-antagonist muscles. Due to the rhythmic auditory signals activating the motor neuronal spinal nuclei through the reticulospinal pathway, metronome-based interventions train the coordination of axial and proximal movements by motor commands. This increased excitability on this pathway decreases muscle reaction time to improve volitional mobility during functional performance.
Handwriting and Metronome Training
Product
Activity Comments
- This activity can be completed with any lined paper and writing utensil – for convenience, laminating lined paper and using a dry erase marker has proved ideal for BOT!
- Typically, we begin with zig-zag lines, every beat of the metronome the patient should either be touching the top line or the bottom line
- Emphasize wrist and finger fluidity – ensure your patient keeps their forearm on the table!
Sample Documentation
The patient completed digit isolation and handwriting tasks in today’s session with the use of metronome in order to provide the potential to regain or improve function through the strengthening of neural pathways for increased efficiency through accurate timing of neuronal firing in the nervous system which is necessary for every process within the brain, whether it is cognitive or motoric. The patient is noted to have difficulty with digit isolation and distal digit fluidity. VC were provided to ensure the ulnar side of the forearm remained anchored to the table. Metronome was set at [55 BPM] and decreased to [50 BPM] for achievability. The patient performed a [total of 4 lines.] The patient stated that it was difficult towards the end d/t fatigue.
Modified Ski Jumping or Dynamic Hopping for Functional Ambulation
Product
Activity Comments
- Place your cones in a zig-zag pattern
- Demonstrate safe completion of this task to your patient
- Start with diagonal lunges and slowly increase to jumps as the patient grows in confidence
Sample Documentation
The patient engaged in a multi-modal diagonal hop-to ambulation pattern around cones placed [14-18″] apart while maintaining balance and postural alignment in rhythmic coordination to a metronome at [56-75bpm]. This task is purposed to elicit and improve agility, movement absorption, eye-foot, eye-hand coordination, visual spatial awareness, gross Strengthening, improved postural alignment during functional ambulation, and dynamic standing balance resulting in greater perceived confidence in ability to be independent and increased self-sufficiency in ADLs and IADLs requiring the aforementioned performance skills. The patient demonstrated hesitancy at first, but increased in dynamic mobility and confidence by the end of the activity which was broken up into two parts, separated by modified jogging. Each set required clearance of approximately [9 cones] over [20ft] and consisted of approximately [4-6 sets.] The patient reports this is a good challenge.
Obstacle Course with Aerobic Steppers and Hurdles
Product
Activity Comments
- This is a higher level obstacle course d/t added challenge of ankle weights and bilateral kettlebell holds
Emphasize slow, controlled, intentional movements
Sample Documentation
The patient engaged in an obstacle course designed with alternating [4] hurdles with 6″ rise 2″ run and [4] aerobic steps 8″ rise by 13″ run to simulate various obstacles required during continuous community mobility. Task requiring verbal cues to correct kyphotic posture and out-toeing through activity in order to encourage normalized gait pattern and decrease risk of static malalignment. The patient completed hurdles and [20 ft] fast walking for [10 sets] while carrying [5lb] kettlebell in BUE and wearing [1.5lb] ankle weights on BLE to increase body schema, generalized strength, and proprioceptive awareness.
Pitch Back Activities
Product
Activity Comments
- Allow your patient to familiarize themselves with the pitchback by having them practice with a weightless ball first
- This task was graded up by placing the patient on an unstable surface (foam pad/rocker board)
- You can also have your client alternate between BUE for catch/release sequence.
- You may give a pattern for catch release (Catch right- right- left, Throw left – left- right)
Sample Documentation
The patient engaged in dynamic standing activity requiring the propulsion of weighted balls [16oz, 18oz, 20oz] from [8ft] away to a pitchback altering between objects for recognition and enhancement of modulation ability. The task was performed [2×25 reps] while alternating between right and left extremity enhancing BUE strength and range of motion, forearm strength, functional grasp/intrinsic strength, reaction time, force absorption through palm and wrist joint, balance, postural alignment, gross muscle stamina, and endurance for activity. [3 sets of 2×25] were performed while standing on various platforms including an unstable balance pad and rocker board. The patient was able to achieve this activity but displayed signs and symptoms of fatigue throughout progression. Therapeutic rest offered between each step to prevent muscle fatigue and episodes of imbalance.
Pinch Strength – Functional Movement and Activity
Product
Activity Comments
- Have your patient seated at a table (consider ergonomics of hand therapy)
- Ensure your patient isn’t compensating higher up in the kinetic chain! Watch for shoulder abduction and trunk flexion
Sample Documentation
The patient engaged in a seated fine motor activity requiring patient to use alternating tip pinch, 3 point pinch, and lateral pinch prehension skills to secure clips [varying levels of resistance] to small objects [x25] with right hand in order to increase intrinsic hand strength, thumb strength, pinch strength, fine motor coordination, and general pain-free mobility. Good challenge. Fatigue noted and observed by the end of the task. No discomfort noted.
Rhythmic Recall – Hand Clapping
Product
Activity Comments
This is a seated task and can be completed as “interference” when engaging a patient in other cognitive tasks!
You can also use this as a primary activity. Ensure that you are able to remember the pattern you are giving to your client! This is great for working on praxis and sustained attention
Sample Documentation
The patient engaged in a rhythmic recall and repeat activity requiring the processing of a clapping rhythm requiring dynamic BUE engagement while seated presented by the therapist. The rhythms varied between [6-10 beats/movements for a total 15 reps.] The patient demonstrated [4/15 rhythms] accurately with greater difficulty noticed beyond 6 movements/beats per rep. Due to the nature of the patient’s dx and the decreasing ability to perform movement during a cognitive-demanding activity, this task is purposed to encourage neuronal activation in the basal ganglionic center / putamen which is said to assist an individual in the registration and interpretation of rhythmic phenomenon required to maintain internal rhythm as well as internal rhythm used for essential activities of life including respiration, ambulation, and the performance of activities requiring BUE and BLE mobility while thinking.
Rolling Medicine Ball Across the Table
Product
Activity Comments
This is an activity that we utilize in moderate stages of ADRD to invoke sustained attention, hand-eye coordination, and reaction time!
You can also use this activity for a variety of other BUE or UE conditioning/mobility restorative continuums.
Sample Documentation
The patient engaged in a dynamic standing activity requiring standing in front of a waist-high table, approximately [4ft in length], and rolling a [6lb] ball across table to therapist [2×25 times] requiring sustained attention to task, “push” mechanics, alignment, eye-hand coordination to receive ball, and initiation of task to push ball back to therapist. The patient was noted to require verbal cues to remain focused on the task [x3]. Pt reacted well to the activity.
Side Stepping Activity
Product
Activity Comments
Helpful Hints:
- If your patient is unable to keep their feet parallel, grade this task down to stepping out and back to midline (rather than stepping 20ft)
- Tactile cues can be helpful to promote proper form and muscle isolation. Get on the floor and guide your patient’s foot where it should be!
- Use VISUAL feedback via mirror so the patient has knowledge of performance
Sample Documentation
The patient engaged in dynamic ambulation activity requiring side stepping [20ftx4] trials with control and proper body mechanics to prevent compensatory strategies in ankle positioning and out toeing. Masking tape strips 12inches apart were placed on the ground as visual cue and refined motor calibration. The patient required [3-4 verbal cues] to pace and execute slow and methodical intentional stepping in order to improve gross muscle activation, motor unit of agonist and antagonist muscles in order to elicit balanced muscle activation during mobility. The patient demonstrated improvement in coordination throughout functional activities.
Theraputty for Functional Movement Patterns of the Hand
Product
Activity Comments
Helpful Hints:
- Ensure you research and print an HEP for your patient prior to sitting down and instructing your patient on how to use Theraputty for hand strengthening.
- Patient education is very important when using this tool
Sample Documentation
The patient engaged in theraputty activity routine using ‘soft’ resistance to address fine motor deficits and intrinsic muscle weakness resulting in a decreased ability to participate in essential acts requiring prehension, coordination, and fine motor skills like patient defined occupations of writing and meal preparation. The patient was required to do [10 reps] of each exercise including finger scissor, finger spread, fingertip pinch, flat pinch, power grip, finger extension, and full grip. The patient engaged in a therapist-initiated [30s-60s] rest between each exercise to prevent muscle fatigue. No c/o pain or discomfort noted.
Upper Extremity Functional Movement Pattern for Donning and Doffing Bra
Product
Activity Comments
- The therapist is positioned behind the patient during this task
- Grasp a tennis ball sized ball and task your patient with pulling it away
- Slightly vary the position of the ball and repeat as many times as necessary
Sample Documentation
The patient engaged in functional movement pattern strengthening activity. The task required the patient to retrieve [x9] [16, 18, and 20 oz] weighted balls from the middle of her back. The patient was given additional therapist provided resistance in order for a just-right challenge. The movement pattern invoked shoulder extension, internal rotation, and adduction, forearm flexion, pronation/supination, and wrist and digit flexion and extension. This activity is purposed to improve strength and activity tolerance through repetition and progressive overload in order to increase participation in daily activities such as UB dressing and decrease pain.
Exercise Ball – Dual Tasking Ball Bounces
Product
Activity Comments
- Ensure your patient is independent with balance, or provide necessary CGA
- Explain to your patient that with each bounce of the ball you will alternate counting backward or forward from a specified number BY a specified number (e.g. count back by 7’s starting at 150)
Sample Documentation
The patient engaged in a catch/release task with medium-sized lightweight ball in variable transfer styles including bouncing and throwing at multiple heights while simultaneously alternating counts [every other digit until 100]. This task was used to increase postural support, reaction time, neuromuscular communication, simultaneous motor unit recruitment in BUE, and establishment of strong BOS, ability to maintain COG over BOS, and the ability to perform dual task activities requiring the performance of executive functions and mobility based tasks. The patient required multiple verbal cues to ensure directions were correct and increased confidence throughout the task. [The patient displayed no difficulties in manipulating numbers nor did she experience LOB.]
Dynamic Reaching with Posterior Gaze Shifting
Product
Activity Comments
- This activity was completed in front of a door (ensured to be not in use) in order to secure the theraband
- The patient was tasked with maintaining balance on the foam pad, grasping the theraband, turning neck, shoulders, and trunk, while simultaneously pulling the theraband from overhead to opposite hip.
Think of the vestibular implicants to this activity!
Sample Documentation
The patient engaged in activity requiring him to stand on a balance pad [uneven surface] with BLE to evoke balance and righting reaction while reaching upward and crossing midline to retrieve yellow theraband. Once yellow theraband secured in grasp, the patient was required to shift his gaze posteriorly, return to forward, and complete cross-midline resistance training. [10 reps each side]. This task is used to improve the patient’s ability to maintain balance while reaching up into cupboards which he identified to be a challenge for him. [x20 reps per side were completed in today’s session]
Bosu Ball with Weighted Ball
Product
Activity Comments
- You should establish your patient’s efficient dynamic balance and fair ankle stability prior to the completion of this activity
- Have an out! Make sure there is an external balance support within reaching distance from your patient (e.g. a chair placed anteriorly to the patient- this will also help your patient get on and off of the bosu ball)
Sample Documentation
The patient engaged in a dynamic balance activity requiring anticipatory postural movements to adapt to BLE placement on the dome of a BOSU Ball. Activity used to improve motor calibration and coordination, as well as amplify abilities of weight-shift, ankle joint stability, and overall control. The patient remained on BOSU throughout isometric activity requiring simultaneous bilateral knee flexion while holding a [4lb weighted ball x10.] The patient performed this task [x2] with the ball, and dynamic standing balance only [x1 minute each.] The patient was not observed to experience LOB, and defined activity as a good challenge. He required a rest break after each set.
Bosu Ball for Weight Shifting and Postural Alignment
Product
Activity Comments
- You should establish your patient’s efficient dynamic balance and fair ankle stability prior to the completion of this activity
- Have an out! Make sure there is an external balance support within reaching distance from your patient (e.g. a chair placed anteriorly to the patient- this will also help your patient get on and off of the bosu ball)
- If you have the option – have a rehab aid toss the ball to your patient while you provide CGA. Even for the most balanced patient this is a very challenging task
Sample Documentation
The patient engaged in a dynamic balance activity requiring BLE placement on a BOSU Ball requiring good balance, good weight-shift, ankle stability, coordination, and control. The patient remained on BOSU throughout catch/release activity [2×50 reps] with [4lb weighted ball] thrown outside BOS alternating sides. The patient was not observed to experience LOB, and defined activity as a good challenge.
Bosu Ball with Gaze Shifting
Product
Activity Comments
- You should establish your patient’s efficient dynamic balance and fair ankle stability prior to the completion of this activity
- Have an out! Make sure there is an external balance support within reaching distance from your patient (e.g. a chair placed anteriorly to the patient- this will also help your patient get on and off of the bosu ball)
- This is a graded up version of the same activity that had the patient positioned on a foam pad
Sample Documentation
The patient engaged in a dynamic balance activity requiring BLE placement on a BOSU Ball requiring good balance, good weight-shift, ankle stability, coordination, and control. The patient was required to maintain COG over BOS while reaching upward and crossing midline to retrieve yellow theraband. Once yellow theraband secured in grasp, the patient was required to shift his gaze posteriorly, return to forward, and complete cross-midline resistance training. [10 reps each arm] while alternating BUE to promote cross-midline intersection. The patient was not observed to experience LOB, and defined activity as a good challenge. The patient requires good dynamic balance with reaction time and coordination during simultaneous BUE activity in order to return to work post injury. [Work Conditioning]
Exercise Ball – Gross Mobility Ball Bounces
Product
Activity Comments
- Ensure your patient is independent with balance, or provide necessary CGA
- Alternate bounces from across the clinic
Sample Documentation
The patient engaged in an unsupported standing dynamic activity requiring the ability to bounce a large exercise ball back forth across room [x50] without self-initiated break in order to increase postural control, core stability, dynamic standing balance, establishment of strong BOS, ability to right COG over BOS despite external stressors and distractions, and increase overall BUE strengthening. Activity utilized to enhance patient’s ability to participate in shower activity without access to essential adaptive equipment, dressing at edge of bed, and BUE engagement over a sustained period of time without premature onset of fatigue.
Upper Extremity Grasp/Release with Midline Crossing
Product
Activity Comments
- Set your patient up in a high back chair, on the mat table, or even standing
- Hold the ring/cone on the opposite side of the patient’s body and task them with retrieving it and releasing it in a designated area
Sample Documentation
The patient engaged in a grasp and release activity in today’s session emphasizing principles of interhemispheric communication by way of continuous midline crossing in order to promote neural excitation, UE strength, ROM, motor initiation, motor termination, and calibration of UE movements. The patient was set up in a high-back chair and was tasked with grasping the ring and placing it around the cone at the opposite side of her body. The patient completed [3×12] repetitions in today’s session. The patient was noted to experience dysmetria when grasping the ring as well as bradykinesia throughout this activity. The patient required rest breaks between each round d/t complaints of LUE fatigue.
Tabletop Upper Extremity Bean Bag Slides with TENS Unit
Product
Activity Comments
- Whenever you utilize a TENS unit ensure you are documenting electrode placement and the settings that were used
- Target muscles that are used in the action you are trying to perform
- A strong recommendation is to invest in a great functional anatomy textbook like “The Trail Guide to the Body”.
Sample Documentation
The patient collaborates with the occupational therapist to apply and utilize TENS unit with targets placed on LUE shoulder flexion prime mover anterior deltoid and synergistic mover coracobrachialis [300 Volts / 2.5 power] in order to elicit an amplified recruitment of motor units and increase motor learning and provide increase muscle activation throughout weaker muscle segments. The patient responded well to intervention without c/o of discomfort. TENS unit used during bean bag activity requiring passive placement of LUE in abduction, external rotation, and pronation with encouragement for AROM in supination, horizontal adduction, and internal rotation after performing a [5 second isometric contraction] of MCP flexion while holding a beanbag. [x35 repetitions] completed. Using TENS resulted in favorable outcomes, though minimal. Therapist provided proprioceptive feedback and physical cue for compensatory movements of neck and trunk lateral flexion.
Bean Bag Toss through Hula Hoop
Product
Activity Comments
Helpful Hints:
- We use this activity and similar ones for later stages of ADRD
- Great for attention, visual tracking/attention, reaction time, hand-eye coordination, etc
- Consider the cues you’re using! Use visual demonstration and short, concise verbal commands
Sample Documentation
The patient engaged in a dynamic unsupported seated activity requiring him to toss a bean bag through a hoop approximately 6 feet off the ground suspended from the ceiling. The task utilized to encourage/elicit neck extension, strong posture, movement/task initiation, eye/hand coordination, modulation, and sustained attention to task. The patient required moderate verbal cues through activity to complete requirements of task and was able to successfully accomplish an accurate toss [5/15 attempts].
Balloon Batting with Bar
Product
Activity Comments
Helpful Hints:
- We use this activity and similar ones for later stages of ADRD
- If there are two people available, position your patient on the edge of a mat table to also address core stability/strength and postural reactions (use NDT facilitation to provide necessary support to your patient – hands on pelvis)
- Great for attention, visual tracking/attention, reaction time, hand-eye coordination, etc
Sample Documentation
The patient engaged in edge of seat dynamic activity using a balloon to elicit alternating RUE and LUE engagement with unsupported trunk [x50] repetitions to increase postural control, core stability, righting reaction during bed mobility, bathing and dressing at edge of bed
Sitting on Balance Disc
Product
Activity Comments
- Balance disc can be set up on a chair or a mat table
- Ensure your patient’s feet can fully touch the ground
- Engage your patient is dynamic UB movements!
Sample Documentation
Patient engaged in an unsupported seated dynamic balance training utilizing balance disk and engaging in alternating lateral trunk flexion repetitions with return to midline [x10 each side] and alternating BUE punches crossing midline [x15 each side] to challenge and strengthen trunk and back musculature, initiate controlled movement, maintain postural alignment and COG over BOS, excite neural pathways when moving in diagonal patterns and crossing midline, and strengthen BUE to support increase patient’s ability to use chairs without armrests at home and community without fear of falling.
Ipsilateral Cone-Tapping
Product
Activity Comments
Helpful Hints:
- Single leg balance can be a disconcerting experience for many patients. Provide CGA/MIN A as necessary as well as external balance aids as the patient gains confidence (chair/parallel bars, etc)
- Emphasize SLOW movements! Patient will typically want to rush through something when they feel unbalanced which works against them and is unsafe
Sample Documentation
The patient engaged in dynamic standing activity requiring unilateral LE balance over [1 second] while performing a toe-tapping activity to reach the target for the purpose of increasing BLE modulation and eye foot coordination during functional mobility activities. The patient was not able to perform greater than [1 second] unilateral LE stance demonstrating atypical weightshift, but was noted to complete the task successfully using rhythmic coordination of metronome at [60 BPM]. The patient required moderate education and verbal cueing for auditory processing and motor praxis
Backward Walking [ Retropedal Ambulation]
Product
Activity Comments
Helpful Hints:
- Backward walking is hugely important! Many falls result in those few functional backward steps (backing up towards a chair or the toilet)
- This activity challenges every body system required in walking minus the visual system (which is why it seems more intimidating to patient’s because they can’t see where they’re going)
- It also emphasizes body schema and spatial awareness. Set up some colored behind your patient, ask them to locate one of them over their shoulder, then have them slowly walk backward until they feel like they’re in line with the cone they identified.
- Use NDT to guide your patient backward! Place your hands on their iliac crests.
Sample Documentation
The patient engaged in a functional ambulation task in today’s session in order to address necessary components of safe movement including body scheme, proprioception, kinesthesia, visual spatial reasoning and awareness, and motor planning all utilized and required in ADLs such as toileting. The patient was tasked with backward walking with therapist facilitation/ provided CGA through the pelvis as a key point of control. The patient was asked to gaze over the left or right shoulder in order to locate a colored cone, return head to midline, and step backward until she felt she was in line with the colored cone identified at the beginning of the trial. The patient required [x6 VC] to only look at the cone once. The patient completed [x7 repetitions] of the exercise and stated that it was a good and appropriate challenge at the completion of said exercise.
Ambulation Over Hurdles [Aerobic Steppers]
Product
Activity Comments
Helpful Hints:
- Emphasize slow and controlled movement!
- Watch for out-toeing and other dysfunction in the lower kinetic chain
Sample Documentation
The patient engaged in functional ambulation training with [3] intermittent hurdles (aerobic steppers) for a total of [200ft] with [2.5 minute rest breaks] every [50ft]. The patient was required to ascend and descend a total of [9 hurdles] with MOD A throughout the task. The patient demonstrated muscle imbalances throughout the pelvic region creating an atypical gait pattern requiring verbal and tactile cues to correct throughout the task.
Obstacle Course for Dementia [One]
Product
Activity Comments
Helpful Hints:
- This obstacle course is modified and used for those diagnosed with ADRD
Therapeutic use of self is very important! Many diagnoses such as Lewy Body Dementia require/ benefit from visual demonstration of tasks. Use tactile cueing and trialing many different verbal cues will be of benefit. A patient that BOT worked with for over a year responded well to continuous tactile cue via therapist hand on lateral aspect of trunk (walking beside him with an arm around his back) as well as commands such as “walk with me”. Think short and concise when it comes to verbal cueing!
Sample Documentation
The patient engaged in a dual tasking obstacle course designed with alternating [3] hurdles with 6″ rise 2″ run and [3] aerobic steps 8″ rise by 13″ run to simulate various obstacles required during continuous community mobility. The patient was given [2-4 instructions varying between difficulty of single step and multi-step commands] in order to assess and enhance working memory, topographical orientation, selective attention, sustained attention, and emotional regulation under pressure.
Figure 8 and Balance Obstacle Course
Product
Activity Comments
Helpful Hints:
- For motor planning, have the patient compete revolutions in their dominant and/or non-affected hand first
- The goal is to complete revolutions without the balls touching each other – this is very difficult!
- We always encourage our patient’s to purchase these balls so they can maximize practice at home while they engage in something leisurely
Sample Documentation
The patient engaged in Baoding balls [2×2-minute] intervals in the left hand to promote intrinsic muscle strength, stability and control of the radiocarpal joint. The activity is designed to promote muscle isolation, manipulation, passive tendon glides, and muscle stamina/endurance of the left hand to promote engagement in functional activities requiring object manipulation using prehension. The patient completed [25 revolutions]
Occupational Therapy Treatment and Documentation Examples
Alzheimer’s Disease Medications
Dementia Treatments Alzheimer's Disease MedicationIntroduction People are increasingly interested in the latest advancements in Alzheimer's disease medications as they seek to safeguard their brain health through the most cutting-edge scientific developments....
The Neurological Therapist – Interview your therapist
One crucial aspect of our practice is understanding the nuances between different treatment modalities and knowing when to apply each one effectively.
Understanding the Difference: Therapeutic Exercise, Therapeutic Activity, and Neuromuscular Re-education in Occupational Therapy
One crucial aspect of our practice is understanding the nuances between different treatment modalities and knowing when to apply each one effectively.
Stages of Alzheimer’s Disease
Alzheimer’s disease progresses through several stages, each presenting its own set of challenges for both the individual and their loved ones. In the early stages, memory lapses and difficulty with familiar tasks may be subtle, but as the disease advances, symptoms become more pronounced. In the middle stages, confusion and disorientation become more frequent, and individuals may require assistance with daily activities. Finally, in the late stages, communication becomes extremely limited, and round-the-clock care is often necessary. Understanding these stages can help families better navigate the journey of Alzheimer’s, providing support and planning for the road ahead.
Warning Signs of Dementia
It is difficult to tell the difference between memory loss in normal aging and warning signs of dementia, but there are several common findings that may serve as a warning sign that something deeper may be happening than normal aging.
Early Signs of Dementia in Women
“Memory is the treasure house of the mind wherein the monuments thereof are kept and preserved”. Thomas Fuller Early signs of dementia in women:Early: This refers to the beginning stages or the initial phase of something. In the context of "early signs of dementia,"...
Traumatic Brain Injury Rehabilitation
Traumatic Brain Injury Rehabilitation Authored by Michelle Eliason, MS, OTR/L, CKTS, C.D.S.What is a Traumatic Brain Injury (TBI)A traumatic brain injury (TBI) can occur after a fall, sport injury, motor vehicle accident, blunt force trauma, accident at work, or any...
Lewy Body Dementia and Rehabilitation
Lewy Body Dementia and Rehabilitation Authored by Michelle Eliason, MS, OTR/L, CKTS, C.D.S.What is Lewy Body Dementia?Lewy Body Dementia (LBD) is the second most prevalent progressive neurodegenerative diagnosis causing dementia. It is second to Alzheimer's disease...
Multiple Sclerosis and Rehabilitation
Multiple Sclerosis and Rehabilitation Authored by Michelle Eliason, MS, OTR/L, CKTS, C.D.S.Common Symptoms of Multiple SclerosisMultiple sclerosis (MS) is a neurodegenerative disease affecting the central nervous system (brain and spinal cord). During the progression...
Parkinson’s Disease
Parkinson's Disease Treatment Parkinson's Disease Therapy and Management Parkinson's Disease treatment; Parkinson's Disease therapy; PD; Parkinson's Physical TherapyCommon Symptoms of Parkinson's DiseaseParkinson's disease is the second most common neurodegenerative...
Alzheimer’s Disease Medications
Dementia Treatments Alzheimer's Disease MedicationIntroduction People are increasingly interested in the latest advancements in Alzheimer's disease medications as they seek to safeguard their brain health through the most cutting-edge scientific developments....
The Neurological Therapist – Interview your therapist
One crucial aspect of our practice is understanding the nuances between different treatment modalities and knowing when to apply each one effectively.
Understanding the Difference: Therapeutic Exercise, Therapeutic Activity, and Neuromuscular Re-education in Occupational Therapy
One crucial aspect of our practice is understanding the nuances between different treatment modalities and knowing when to apply each one effectively.
Stages of Alzheimer’s Disease
Alzheimer’s disease progresses through several stages, each presenting its own set of challenges for both the individual and their loved ones. In the early stages, memory lapses and difficulty with familiar tasks may be subtle, but as the disease advances, symptoms become more pronounced. In the middle stages, confusion and disorientation become more frequent, and individuals may require assistance with daily activities. Finally, in the late stages, communication becomes extremely limited, and round-the-clock care is often necessary. Understanding these stages can help families better navigate the journey of Alzheimer’s, providing support and planning for the road ahead.
Warning Signs of Dementia
It is difficult to tell the difference between memory loss in normal aging and warning signs of dementia, but there are several common findings that may serve as a warning sign that something deeper may be happening than normal aging.
Early Signs of Dementia in Women
“Memory is the treasure house of the mind wherein the monuments thereof are kept and preserved”. Thomas Fuller Early signs of dementia in women:Early: This refers to the beginning stages or the initial phase of something. In the context of "early signs of dementia,"...
Traumatic Brain Injury Rehabilitation
Traumatic Brain Injury Rehabilitation Authored by Michelle Eliason, MS, OTR/L, CKTS, C.D.S.What is a Traumatic Brain Injury (TBI)A traumatic brain injury (TBI) can occur after a fall, sport injury, motor vehicle accident, blunt force trauma, accident at work, or any...
Lewy Body Dementia and Rehabilitation
Lewy Body Dementia and Rehabilitation Authored by Michelle Eliason, MS, OTR/L, CKTS, C.D.S.What is Lewy Body Dementia?Lewy Body Dementia (LBD) is the second most prevalent progressive neurodegenerative diagnosis causing dementia. It is second to Alzheimer's disease...
Multiple Sclerosis and Rehabilitation
Multiple Sclerosis and Rehabilitation Authored by Michelle Eliason, MS, OTR/L, CKTS, C.D.S.Common Symptoms of Multiple SclerosisMultiple sclerosis (MS) is a neurodegenerative disease affecting the central nervous system (brain and spinal cord). During the progression...
Parkinson’s Disease
Parkinson's Disease Treatment Parkinson's Disease Therapy and Management Parkinson's Disease treatment; Parkinson's Disease therapy; PD; Parkinson's Physical TherapyCommon Symptoms of Parkinson's DiseaseParkinson's disease is the second most common neurodegenerative...