SOAP Note for Occupational Therapy
{Discharge Notes}
Stop feeling insecure and lost.
Don't wait for BURNOUT to consume your life because there just isn't enough time for professional development or searching for evidence-based information and training for daily clinical treatments.
Join the BOT Rehabilitation Resource Portal and Receive 24/7 access to the highest quality resources designed by an experienced therapist speciically for busy, motivated, and passionate therapists and therapy assistants.

Membership Perks
What is included?
Your investment gives you resources to save you stress, self-doubt, and burnout as you become a confident and competent practitioner who can stand up for your professional point of view and scope of practice.
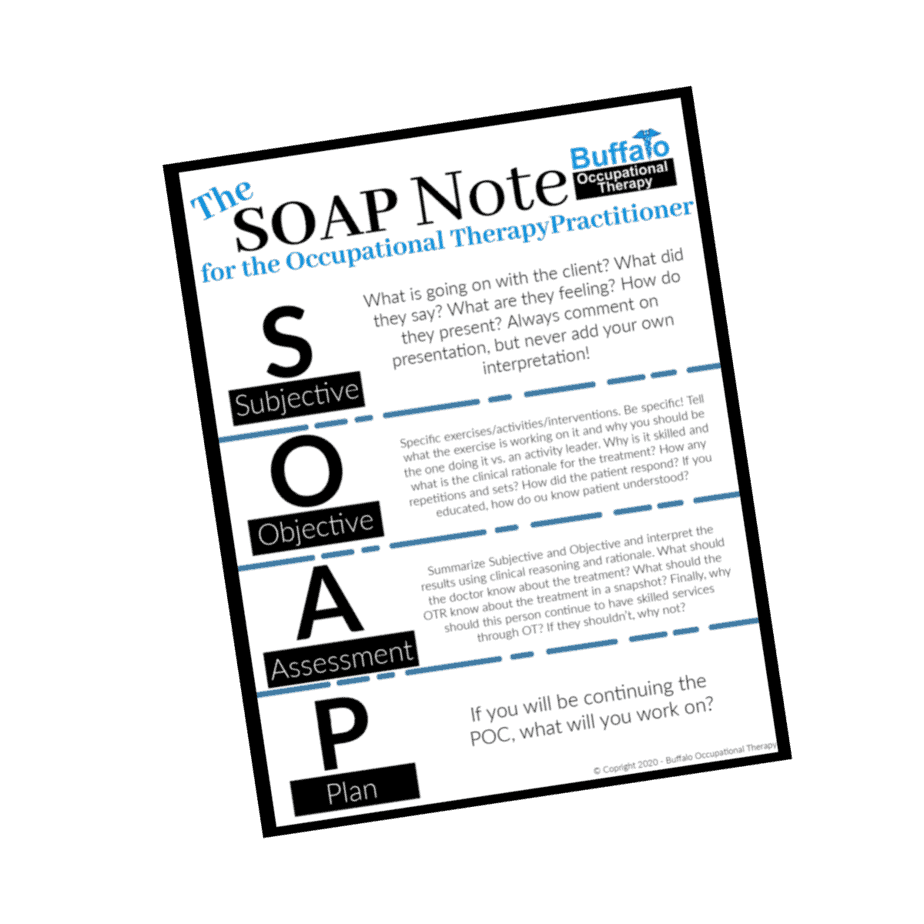
SOAP Notes for Occupational Therapy discharge notes are a time where you can complete your patient’s story and write their next chapter! Depending on the setting you are in and the electronic medical records system they are using for documentation, the format of your SOAP discharge note may be different—but the general execution should remain the same.
General Guidelines
S = Subjective
O = Objective
A = Assessment
P = Plan
S
As always, the subjective section of a discharge note is not open for interpretation. This is completely patient feedback. Take time to interview your client and debrief.
- How do you feel about the conclusion of your plan of care with OT?
- Have your goals been met? Do you have persisting questions or concerns?
- What do you feel are your next steps?
- Based on where you started, how do you feel you have improved?
O
Update your objective measures. This section of the discharge note contains all of your baseline measurements. This is just like your progress note. The following assessments are examples of what assessments you can update in your progress note: MMT, ROM, BERG, DASH, TUG, 9 hole peg, SLUMS, ABC Balance Confidence Scale, etc.
As you update these objective measures, consider what it means. How are you going to interpret these outcomes? Has your patient improved, declined, or remained the same? Did they meet their goals? If they have not met their goals, consider why. Also consider why they are being discharged if they haven’t met their goals. Is it an appropriate discharge? All of this information must be interpreted and addressed in the next two sections of your SOAP discharge note.
Remember that this section does not have feelings or interpretation!! This is the data. This is rigid, black and white information.
A
Summarize Subjective and Objective sections of your progress note and interpret the results using clinical reasoning and rationale.
- What should the doctor know about the culmination of this plan of care?
- What should the patient know about the culmination of this plan of care? (Remember, they can read these documents as well!)
- What gains have they made? How have they declined or remained the same?Summarize your objective measures.
- Have new barriers presented themselves which impact therapeutic potential?
P
Provide brief next steps. What is the patient’s next step in the continuum of care? Are future therapies recommended? Why or why not? If so, what would you recommend the next therapist address? If your loved one was disengaging, what would you want them to know?
Browse the Resource Store!
Don't want to pay for each PDF individually? No problem! The BOT Portal Membership comes with all printable resources and more!